Ethical Debate Topics in Nursing: Top Controversial Ethical Topics Every Nurse Should Know on Ethics
Nursing practice exists at the intersection of clinical science, human values, and professional responsibility. Every day, nurses make decisions that extend beyond technical competence, requiring careful judgment about what ought to be done in situations where outcomes are uncertain, values may conflict, and the stakes are profoundly human. These moments arise in routine bedside care as well as in highly complex clinical scenarios, shaping how nurses advocate for patients, collaborate with interdisciplinary teams, and uphold professional standards.
As healthcare systems evolve, nurses are increasingly confronted with situations that demand thoughtful reflection and reasoned discussion rather than simple right-or-wrong answers. Advances in medical technology, shifting societal expectations, and growing diversity in patient populations have expanded the range of questions nurses must navigate. Whether balancing respect for individual preferences with public safety, responding to family disagreements, or adapting to new decision-making tools in clinical environments, nurses must be prepared to think critically and articulate well-reasoned positions.
Structured debate and ethical reflection play a crucial role in nursing education and professional development. They provide a framework for examining complex scenarios from multiple perspectives, testing assumptions, and clarifying professional responsibilities. Engaging with challenging questions through guided discussion helps nursing students and practicing nurses strengthen judgment, improve communication, and develop the confidence needed to address difficult situations in real-world settings.
This article explores major areas of ethical tension in contemporary nursing practice, drawing attention to situations nurses are most likely to encounter across clinical contexts. By examining real-world examples, established frameworks, and emerging challenges, the discussion aims to support deeper understanding and informed dialogue. For nursing students, educators, and practicing clinicians alike, these discussions are not abstract exercises—they are essential tools for preparing to deliver compassionate, responsible, and accountable care in an increasingly complex healthcare landscape.
What are the most pressing ethical issues in nursing practice today?
Nursing practice increasingly involves complex decision-making that goes beyond clinical skills and technical knowledge. Nurses work in environments where patient needs, institutional policies, legal standards, and societal expectations frequently intersect. As a result, they are often required to make difficult judgments in situations where values conflict, outcomes are uncertain, and time is limited. Understanding the most pressing concerns in contemporary practice helps nurses prepare for these challenges and engage in informed, reflective decision-making.
Ethical Issues: Patient Autonomy and Person’s Rights
One of the most significant ethical issues in nursing today involves respecting patient autonomy while safeguarding a person’s rights. Autonomy requires that patients have the freedom to make informed decisions about their own care, including the right to accept or refuse treatment. Nurses play a critical role in upholding this principle by ensuring patients receive accurate information, understand their options, and are supported in expressing their preferences.
Challenges arise when patient decisions conflict with medical recommendations or family expectations. For example, a patient with full decision-making capacity may decline a blood transfusion due to deeply held beliefs. In this situation, the nurse must advocate for the patient’s wishes while also ensuring that the healthcare team understands and respects the decision. This responsibility becomes even more complex when patients have limited health literacy, language barriers, or fluctuating capacity, requiring nurses to carefully assess understanding and involve appropriate supports without undermining autonomy.
Ethical Dilemma: Confidentiality vs. Public Safety
Another major concern in nursing practice emerges when confidentiality conflicts with broader safety considerations, creating an ethical dilemma. Protecting patient privacy is a foundational professional obligation, fostering trust and encouraging open communication between patients and healthcare providers. However, situations may arise in which maintaining confidentiality could place others at significant risk.
For instance, a nurse may learn that a patient poses a credible threat of harm to others or is unwilling to disclose information related to a serious communicable condition. In such cases, nurses must weigh their duty to protect private information against their responsibility to prevent foreseeable harm. These situations often require consultation with supervisors, ethics committees, or legal counsel, as well as careful adherence to institutional and regulatory guidelines to ensure decisions are both professionally and legally defensible.
Moral Dilemmas: Resource Allocation and Triage Decisions
Nurses also encounter moral dilemmas when faced with limited healthcare resources and the need to make triage decisions. Resource allocation challenges are especially pronounced in emergency departments, intensive care units, and disaster or crisis situations, where the demand for care exceeds what is available. Nurses may be required to prioritize patients based on urgency, likelihood of benefit, or established triage protocols.
For example, during large-scale emergencies, nurses may need to delay care for some patients in order to focus on those with the greatest chance of survival. While such decisions are guided by clinical criteria and organizational policies, they can still cause significant emotional distress for nurses who are committed to providing care to all patients. These experiences highlight the moral weight of nursing practice and the importance of institutional support, clear guidelines, and opportunities for reflection after difficult clinical events.
How should nurses approach end-of-life ethics and euthanasia debates?
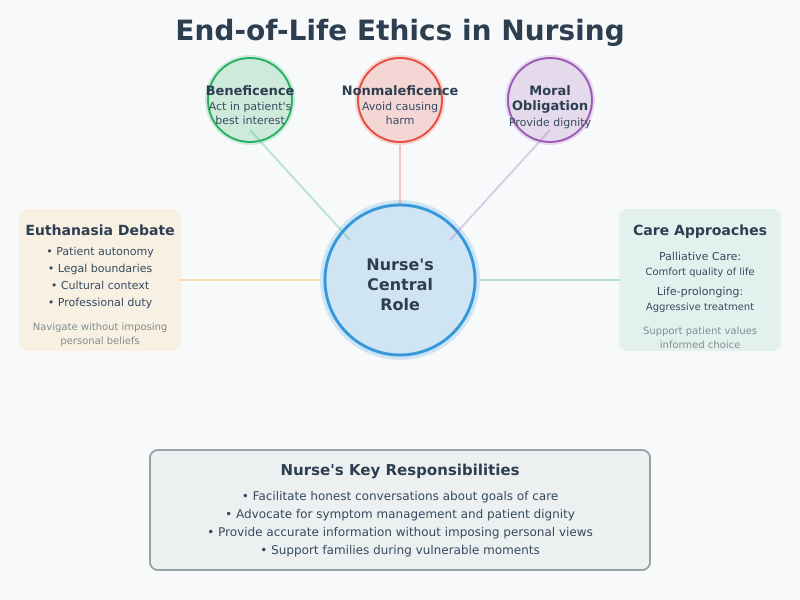
End-of-life care represents one of the most emotionally charged and ethically complex areas of nursing practice. Nurses often serve as the primary point of contact for patients and families during moments of profound vulnerability, making their role central to discussions about comfort, dignity, and treatment goals. Approaching these situations requires sensitivity, professional judgment, and a clear understanding of the ethical foundations that guide nursing practice. Rather than offering definitive answers, nurses must be prepared to engage thoughtfully with competing values, legal boundaries, and deeply personal beliefs.
Euthanasia: Is Physician-assisted Dying Ethically Justifiable?
Debates surrounding euthanasia frequently arise in contexts where suffering persists despite aggressive medical management. The question of whether physician-assisted dying is ethically justifiable remains highly contested within healthcare, shaped by cultural norms, legal frameworks, and professional standards. Nurses, even when not directly involved in decision-making authority, are often closely involved in patient care during these discussions.
For example, a patient experiencing advanced illness with refractory pain may express a desire to hasten death to avoid further suffering. Nurses may find themselves supporting the patient emotionally while also navigating institutional policies that either permit or prohibit such practices. In these situations, the nurse’s role is not to impose personal beliefs, but to provide accurate information, ensure the patient’s concerns are communicated to the healthcare team, and advocate for symptom management options that align with professional and legal guidelines.
Terminally ill: Palliative Care vs. Life-prolonging Treatment
For patients who are terminally ill, decisions often center on whether to prioritize palliative care or continue life-prolonging treatment. This distinction can be difficult for patients and families to understand, particularly when hope for recovery conflicts with medical realities. Nurses play a critical role in clarifying care goals, explaining the purpose of comfort-focused interventions, and supporting shared decision-making.
Consider a patient with advanced cancer who must choose between additional aggressive therapy with limited benefit or a transition to palliative services focused on pain control and quality of life. Nurses frequently help patients articulate what matters most to them—such as comfort, time with family, or avoidance of invasive procedures—and ensure these preferences are respected. By facilitating honest conversations, nurses help align treatment plans with patient values while reducing unnecessary suffering.
Ethical Principles: Beneficence, Nonmaleficence and Moral Obligation
End-of-life decision-making in nursing is grounded in core ethical principles, particularly beneficence, nonmaleficence, and moral obligation. Beneficence emphasizes acting in the patient’s best interests, promoting comfort and well-being even when cure is no longer possible. Nonmaleficence requires nurses to avoid interventions that cause harm, including treatments that prolong suffering without meaningful benefit. Moral obligation reflects the nurse’s duty to provide compassionate care, advocate for patient dignity, and remain present during moments of distress.
In practice, these principles guide nurses when evaluating whether continued intervention serves the patient or merely extends the dying process. For example, administering aggressive treatments that offer minimal improvement may conflict with nonmaleficence, while prioritizing symptom relief and emotional support aligns with beneficence. Nurses must continually reflect on these principles as clinical conditions evolve, recognizing that ethical decision-making at the end of life is dynamic rather than fixed.
What List of ethical questions arise from advances in genetic engineering and gene editing?
Rapid developments in genetics are reshaping modern healthcare, offering new possibilities for preventing disease, personalizing treatment, and improving patient outcomes. At the same time, these advances raise profound questions for nursing practice, particularly around responsibility, consent, and the broader consequences of altering human biology. Nurses, as patient advocates and educators, are increasingly expected to understand these developments and engage thoughtfully in discussions that extend beyond immediate clinical outcomes.
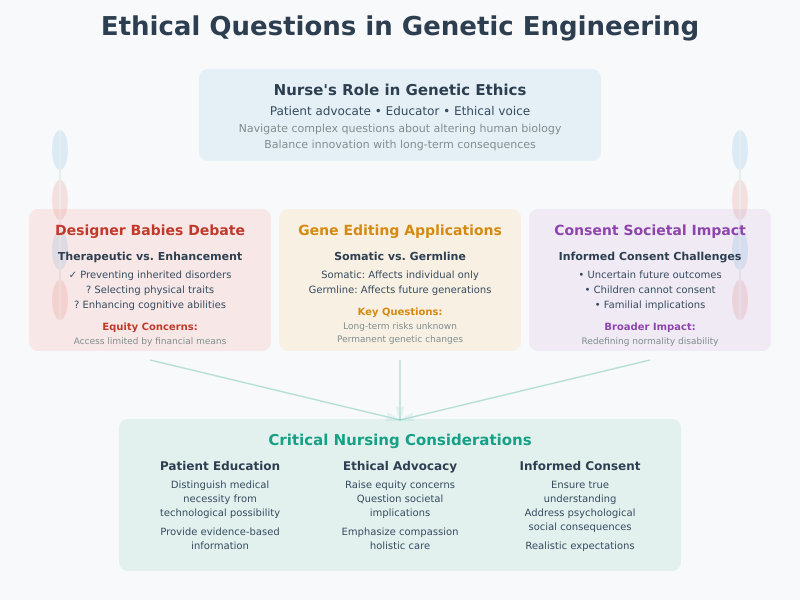
Genetic engineering: ethical debate over designer babies
The use of genetic engineering has sparked significant ethical debate around the concept of “designer babies,” where genetic traits could potentially be selected or enhanced before birth. While current clinical applications are largely focused on preventing serious inherited disorders, the possibility of non-medical enhancements—such as selecting physical traits or cognitive characteristics—raises serious concerns.
From a nursing perspective, this debate highlights issues of equity and fairness. If such technologies become widely available, access may be limited to those with financial means, potentially deepening social inequalities. Nurses involved in prenatal care or genetic counseling may encounter parents who are confused about what is medically appropriate versus what is technologically possible. In these situations, nurses play a key role in providing clear, evidence-based information while reinforcing the distinction between therapeutic interventions and enhancement-driven choices.
Gene editing: justifiable medical uses vs. controversial topics
Advances in gene editing technologies have introduced the possibility of correcting genetic mutations responsible for severe diseases. In cases such as inherited blood disorders or certain metabolic conditions, targeted interventions may be viewed as justifiable because they aim to reduce suffering and improve quality of life. However, these benefits exist alongside controversial topics, particularly when interventions affect future generations or are applied without a full understanding of long-term risks.
For example, editing genes in somatic cells may benefit an individual patient without affecting offspring, whereas germline interventions permanently alter genetic material passed on to future generations. Nurses involved in research settings or specialty clinics may be asked to support patients considering participation in clinical trials. This requires careful explanation of potential benefits, uncertainties, and ethical implications, ensuring patients can make informed decisions without unrealistic expectations.
Ethical to use: consent and long-term societal impacts
A central question in genetic innovation is whether it is ethical to use these technologies when outcomes extend beyond the individual patient. Informed consent becomes especially complex when future risks are unknown or when decisions affect children who cannot consent for themselves. Nurses must consider whether patients truly understand the implications of genetic interventions, including psychological, social, and familial consequences.
Beyond individual consent, there are broader societal impacts to consider. Widespread genetic modification could influence how society defines normality, disability, and responsibility for health outcomes. Nurses, grounded in holistic and patient-centered care, are well positioned to raise concerns about how these technologies might shape public attitudes and healthcare priorities. By engaging in interdisciplinary dialogue, nurses contribute valuable perspectives that emphasize compassion, equity, and long-term well-being.
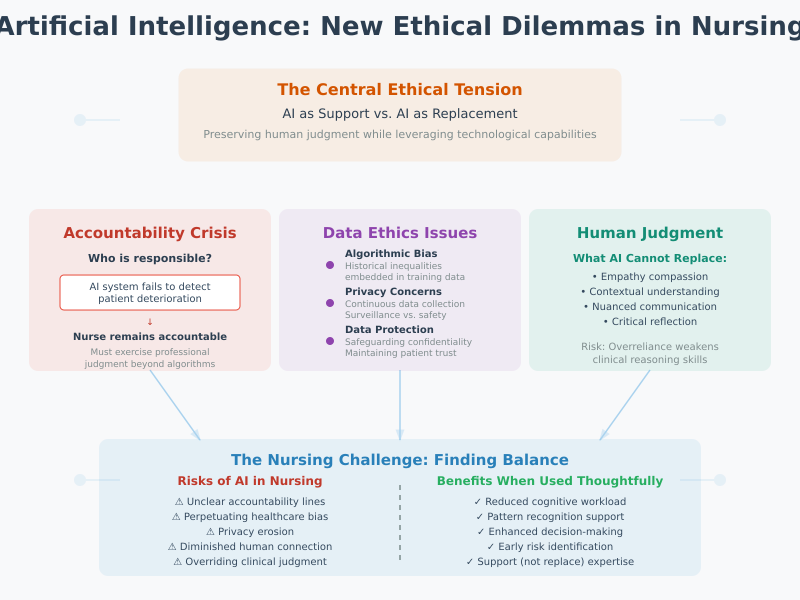
How does artificial intelligence create new ethical dilemmas in nursing?
The integration of digital technologies into healthcare has transformed how nurses assess patients, document care, and support clinical decision-making. Among these innovations, artificial intelligence has emerged as a powerful tool capable of analyzing large volumes of data, predicting risks, and assisting with complex clinical judgments. While these capabilities offer significant potential benefits, they also introduce new forms of ethical tension that directly affect nursing roles, responsibilities, and professional accountability.
Artificial intelligence: accountability for AI-driven decisions
One of the most pressing concerns relates to accountability when clinical decisions are influenced by algorithmic recommendations. As artificial intelligence systems are increasingly used to flag patient deterioration, recommend interventions, or prioritize care, questions arise about who is ultimately responsible for the outcomes of these decisions. Nurses may rely on AI-supported alerts to identify at-risk patients, yet they remain professionally accountable for the care they deliver.
For example, if an AI system fails to identify early signs of sepsis and a patient’s condition worsens, responsibility does not rest with the technology alone. Nurses must still exercise professional judgment, recognize limitations of automated tools, and intervene when clinical observations conflict with algorithmic outputs. This challenge underscores the importance of viewing AI as a support mechanism rather than a substitute for nursing expertise, while maintaining clear lines of accountability within healthcare teams.
Ethics topics: bias, privacy and patient data protection
Several key ethics topics arise from the data-driven nature of AI systems, particularly concerns related to bias, privacy, and patient data protection. AI algorithms are trained on existing datasets, which may reflect historical inequalities or incomplete representations of diverse populations. If these biases are embedded into clinical tools, they can contribute to unequal care outcomes, especially for marginalized or underrepresented groups.
Privacy concerns are equally significant. AI systems often rely on continuous data collection from electronic health records, wearable devices, or monitoring technologies. Nurses are frequently responsible for documenting and managing patient information, placing them at the forefront of safeguarding confidentiality. For instance, the use of predictive analytics to monitor patient behavior may improve safety but also raise concerns about surveillance and consent. Nurses must balance the benefits of data-driven insights with the obligation to protect patient trust and confidentiality.
Ethical debate: replacing human judgement vs. supporting clinicians
A central ethical debate surrounding AI in nursing focuses on whether these technologies risk replacing human judgement or appropriately supporting clinicians. Nursing care is inherently relational, involving empathy, contextual understanding, and nuanced communication—qualities that cannot be fully replicated by algorithms. Overreliance on automated systems may reduce opportunities for critical reflection and weaken clinical reasoning skills.
At the same time, when used thoughtfully, AI can enhance nursing practice by reducing cognitive workload and highlighting patterns that may not be immediately visible. For example, decision-support tools can help nurses manage complex patient assignments or recognize subtle trends in vital signs. The ethical challenge lies in ensuring that AI augments rather than overrides professional judgment, preserving the nurse’s central role in patient-centered care.
Which ethical theories help nurses resolve moral issues at the bedside?
Clinical nursing practice frequently places nurses in situations where competing values, limited information, and emotional stress complicate decision-making. In these moments, ethical reasoning provides a structured way to analyze situations rather than relying solely on intuition or personal beliefs. Ethical frameworks help nurses clarify what is at stake, identify relevant obligations, and justify decisions in a manner consistent with professional standards and patient-centered care.
Ethical theories: virtue ethics and duty-based approaches
Among the most influential ethical theories guiding nursing practice are virtue ethics and duty-based approaches. Virtue ethics emphasizes the character and moral qualities of the nurse rather than focusing solely on rules or outcomes. From this perspective, qualities such as compassion, honesty, courage, and integrity shape ethical action. For example, when caring for a patient who is fearful or distrustful, a nurse guided by virtue ethics prioritizes empathy and trust-building, recognizing that moral action arises from good character as much as from correct procedures.
Duty-based approaches, often associated with moral obligations and professional responsibilities, focus on what nurses are required to do regardless of personal feelings or potential outcomes. In practice, this may involve adhering to professional codes, respecting informed consent, or maintaining confidentiality even when doing so is emotionally difficult. Together, these approaches remind nurses that ethical care involves both who they are as professionals and what they are obligated to do within their roles.
Ethical principles: applying utilitarianism vs. deontology in practice
Clinical decision-making often requires nurses to weigh competing ethical principles, particularly when applying utilitarianism versus deontology in real-world scenarios. Utilitarian thinking focuses on outcomes, aiming to produce the greatest overall benefit for the greatest number of people. In high-pressure settings such as emergency departments, this approach may guide triage decisions where limited resources must be allocated to those most likely to benefit.
In contrast, deontology emphasizes adherence to moral rules and duties, regardless of consequences. From this perspective, each patient deserves respect and fair treatment as an individual, not merely as part of a broader calculation of outcomes. For instance, a nurse may feel tension when institutional efficiency pressures conflict with the duty to spend adequate time addressing a patient’s concerns. Understanding the differences between these approaches helps nurses articulate why certain decisions feel ethically justified, even when no option is entirely free of moral tension.
Critical thinking skills: using ethics frameworks to address dilemmas
Strong critical thinking skills are essential for applying ethical theories effectively at the bedside. Ethics frameworks provide nurses with a systematic method for identifying the core problem, gathering relevant clinical and contextual information, considering stakeholder perspectives, and evaluating possible courses of action. Rather than offering automatic answers, these frameworks encourage reflective analysis and reasoned judgment.
For example, when faced with a patient refusal of treatment, a nurse might use an ethics framework to assess decision-making capacity, consider professional duties, evaluate potential harms and benefits, and consult appropriate resources such as ethics committees or institutional guidelines. This structured process supports consistent, transparent decision-making and helps nurses communicate their reasoning clearly to patients, families, and interdisciplinary teams.
100 engaging debate topics and essay topics for nursing students on ethics
1. Patient Autonomy and Person’s Rights (30 Topics)
- Should patients have the right to refuse life-saving treatment?
- Is informed consent always fully achievable in nursing practice?
- Should minors be allowed to make independent healthcare decisions?
- Are patients ethically obligated to follow medical advice?
- Should families have veto power over a patient’s treatment?
- Balancing autonomy and beneficence: which should prevail?
- Patient rights vs. institutional policies: ethical priorities.
- Should patients have access to all their electronic health records?
- Is it ethical to override a patient’s refusal of medication during mental health crises?
- Respecting cultural beliefs vs. medical recommendations.
- Should patient autonomy include the right to choose alternative medicine?
- Should patients have the right to request assisted suicide?
- How far should nurses go in advocating for patient decisions?
- Is withholding information ever ethically justifiable?
- The ethics of patient-controlled sedation.
- Ethical implications of patient participation in clinical trials.
- Should patients have the right to refuse vaccination?
- Balancing patient autonomy and public health in epidemics.
- The ethics of advance directives.
- Should patients be able to refuse organ transplants if needed?
- Is it ethical to limit patient choices due to resource scarcity?
- How should nurses handle conflicts between patient and family wishes?
- Ethical challenges of respecting patient autonomy in end-of-life care.
- Should autonomy extend to dietary and lifestyle choices in hospitals?
- Patient rights vs. institutional liability: ethical considerations.
- Ethical dilemmas when patient decisions endanger others.
- Consent for minors in reproductive health decisions.
- Should nurses respect patient refusal of pain medication?
- Autonomy and mental competence: ethical boundaries.
- The role of advocacy in protecting patient rights.
2. End-of-Life Ethics and Euthanasia (30 Topics)
- Is physician-assisted dying ethically justifiable?
- Palliative care vs. life-prolonging treatment: which is ethical?
- Should terminally ill patients have the right to refuse nutrition?
- Ethical considerations in Do Not Resuscitate (DNR) orders.
- The ethics of withdrawing life support.
- Should nurses participate in euthanasia if legal?
- Hospice care ethics: balancing comfort vs. prolonging life.
- Moral implications of sedating terminally ill patients.
- Is withholding treatment ethically different from withdrawing it?
- Balancing family wishes and patient autonomy at the end of life.
- Ethical dilemmas in organ donation from terminal patients.
- Should healthcare workers be morally obligated to provide palliative care?
- End-of-life care in resource-limited settings: ethical issues.
- Should nurses follow patients’ advance directives even if they conflict with personal beliefs?
- Ethical concerns with experimental treatments for terminal illnesses.
- Comfort vs. cost: ethical allocation of resources for terminal patients.
- Should terminally ill minors have a say in treatment decisions?
- Is prolonging life always in the patient’s best interest?
- Ethical challenges in withdrawing mechanical ventilation.
- Should pain management take precedence over longevity in terminal care?
- Cultural and religious considerations in end-of-life care.
- Balancing truth-telling and hope in terminal diagnoses.
- Nurse’s moral responsibility in euthanasia debates.
- The ethics of physician-assisted dying in mental illness.
- Should patients have the right to choose their time of death?
- Ethical debates on assisted dying in chronic but non-terminal illness.
- Palliative sedation vs. euthanasia: moral distinctions.
- End-of-life decision-making in incapacitated patients.
- The ethics of life-prolonging interventions for severely disabled patients.
- How should nurses approach ethical disagreements with families?
3. Genetic Engineering and Gene Editing (30 Topics)
- Ethical debate over designer babies.
- Gene editing for disease prevention: justifiable or risky?
- Should gene therapy be used to enhance intelligence?
- Long-term societal impacts of genetic modification.
- Should nurses educate patients on genetic testing risks?
- Consent and ethics in genetic interventions for minors.
- Should parents decide on gene editing for their children?
- Is it ethical to select embryos based on physical traits?
- Gene editing for cosmetic purposes: ethical boundaries.
- Public health vs. individual choice in genetic modification.
- Ethical concerns with CRISPR technology.
- Should gene editing be allowed to prevent inherited diseases?
- Societal inequity in access to genetic therapies.
- Moral responsibility of nurses in genetic counseling.
- Should nurses advocate for ethical limits on gene editing?
- Impact of designer babies on diversity and equality.
- The ethics of prenatal genetic testing.
- Gene editing to prevent disabilities: moral considerations.
- Should genetic modifications be regulated internationally?
- Ethical debate over patenting genetic therapies.
- Can consent be fully informed for experimental genetic interventions?
- Genetic privacy: protecting patients’ DNA data.
- Nurses’ role in supporting patient decisions on genetic therapies.
- Balancing innovation and ethics in gene editing.
- Ethical challenges in somatic vs. germline editing.
- Gene editing and the concept of “playing God.”
- Who decides which traits are desirable?
- Moral dilemmas in experimental gene therapy trials.
- The ethics of correcting genetic diseases in adults.
- How should nurses address family pressure in genetic decisions?
4. Artificial Intelligence and Technology in Nursing (30 Topics)
- Accountability for AI-driven clinical decisions.
- Ethical concerns of replacing human judgment with AI.
- Privacy and patient data protection in AI systems.
- AI bias in clinical decision-making.
- Should nurses rely on AI recommendations without question?
- Ethical debate: AI for predicting patient outcomes.
- Impact of AI on patient trust in nurses.
- Is it ethical to use AI to monitor patient adherence?
- Balancing efficiency and empathy when using AI tools.
- Can AI exacerbate healthcare inequities?
- Nurses’ responsibility for AI errors.
- Ethics of AI-assisted triage in emergency care.
- Confidentiality challenges with AI-powered electronic health records.
- AI in mental health assessment: ethical implications.
- Informed consent for AI-supported interventions.
- Should AI replace routine nursing assessments?
- Ethical concerns in remote AI-driven monitoring.
- Nurses’ role in validating AI recommendations.
- Transparency vs. proprietary AI algorithms: ethical debate.
- Moral dilemmas when AI conflicts with clinical judgment.
- AI and patient autonomy: ethical considerations.
- Should nurses be trained to understand AI limitations?
- Ethical debate: AI in predictive healthcare analytics.
- AI’s impact on nurse-patient communication.
- Moral responsibility in delegating care to AI tools.
- Is AI ethically justified in allocating scarce resources?
- Using AI for patient risk scoring: ethical challenges.
- Ethical issues in integrating AI into long-term care.
- AI and informed decision-making in nursing practice.
- Should AI-supported decisions require human oversight?
Conclusion
Ethical debate and reflection are integral to nursing practice, shaping how nurses navigate complex clinical, technological, and societal challenges. From respecting patient autonomy to grappling with end-of-life decisions, genetic engineering, and the integration of artificial intelligence, nurses are continually called to balance competing values, legal obligations, and professional standards. Understanding ethical principles such as beneficence, nonmaleficence, and moral obligation, and applying ethical theories like virtue ethics, utilitarianism, and deontology, equips nurses with the tools to resolve dilemmas thoughtfully and responsibly.
Engaging with structured ethical debate topics, whether through classroom discussion, reflective exercises, or professional dialogue, strengthens critical thinking skills, enhances patient advocacy, and prepares nursing students to make informed decisions in real-world clinical environments. By confronting moral dilemmas, evaluating ethical questions, and considering controversial topics, nurses can ensure that care delivery remains patient-centered, equitable, and aligned with both professional standards and societal expectations.
Ultimately, cultivating ethical awareness and the ability to reason through challenging situations is not just an academic exercise—it is foundational to the integrity, trust, and effectiveness of the nursing profession. Nurses who actively engage in ethical reflection and debate are better positioned to provide compassionate, responsible, and morally sound care in an increasingly complex healthcare landscape.
Frequently Asked Questions
What are the topics for nursing debate?
Nursing debate topics often focus on patient care, professional responsibility, and healthcare policies. Examples include:
- Mandatory vaccination for healthcare workers
- Patient autonomy vs. family wishes
- Allocation of scarce resources in hospitals
- Nurse involvement in euthanasia or physician-assisted dying
- Use of artificial intelligence in clinical decision-making
- Genetic engineering and designer babies
- Confidentiality vs. public safety
- End-of-life care decisions and palliative vs. life-prolonging treatments
What are the ethical topics of nursing?
Ethical topics in nursing explore principles, dilemmas, and professional conduct, such as:
- Patient autonomy and informed consent
- Beneficence, nonmaleficence, and moral obligation
- Confidentiality and privacy
- End-of-life care and euthanasia debates
- Resource allocation and triage decisions
- Professional accountability and advocacy
- Ethical use of technology and artificial intelligence
- Cultural competence and equitable care
What are some examples of ethical issues in healthcare?
Common ethical issues in healthcare include:
- Confidentiality breaches
- Patient autonomy vs. medical recommendations
- Informed consent and capacity
- End-of-life decision-making
- Allocation of scarce resources
- Conflicts of interest
- Genetic testing and interventions
- Use of experimental treatments
- Bias in care delivery
- Reporting errors or adverse events
What are the 12 ethical issues?
While frameworks may vary, the 12 widely recognized ethical issues in healthcare often include:
- Patient autonomy
- Beneficence
- Nonmaleficence
- Justice (equity in care)
- Confidentiality and privacy
- Informed consent
- End-of-life decision-making
- Allocation of scarce resources
- Professional integrity and accountability
- Conflicts of interest
- Cultural competence and respect for diversity
- Use of emerging technologies (e.g., AI, genetic engineering)
