Best Nursing PICOT Topics and PICOT Question Examples for Evidence-Based Practice
Formulating meaningful and answerable questions is a foundational skill in nursing research and clinical decision-making. In nursing practice, questions often arise from patient care challenges, variations in outcomes, or uncertainty about the most effective nursing intervention. Without a structured approach, these questions can remain too broad, unfocused, or disconnected from available research evidence. This is where the PICOT framework plays a critical role, offering nurses and nursing students a systematic method for translating real-world clinical concerns into focused, researchable clinical questions.
The PICOT approach—widely used in evidence-based nursing—provides a clear structure for developing a well-defined research question by identifying the patient population, intervention, comparison, outcome, and time frame. When applied correctly, a PICOT question supports the research process by guiding literature searches, strengthening study design, and ensuring that the resulting research question aligns with relevant evidence. For nursing students, especially those completing a nursing research assignment or nursing paper, learning how to move from a general background question to a focused PICOT question is essential for academic success and professional development.
Beyond academic requirements, nursing PICOT questions serve an important function in clinical research and everyday patient care. They help healthcare professionals evaluate whether an intervention is effective compared to usual care, standard care, or no intervention, and whether it leads to meaningful health outcomes such as improved pain relief, better blood sugar levels, reduced length of stay, or lower risk of developing complications. By grounding inquiry in evidence-based practice, PICOT questions bridge the gap between nursing research and clinical decision-making.
This article provides a comprehensive exploration of nursing PICOT topic ideas and practical PICOT question examples relevant to modern nursing practice. It examines how the PICOT and PICO frameworks shape focused clinical questions, how nursing students can identify a good PICOT topic, and how common nursing research areas—such as chronic conditions, maternal health, critical care, and patient safety—can be translated into well-built research questions. Through structured guidance and applied examples, the goal is to support nursing students and healthcare providers in developing clear, evidence-based questions that align with both academic standards and real-world clinical needs.

150 PICOT Question Ideas
1. Chronic Disease Management
- Blood glucose monitoring in patients with type 1 diabetes
- Continuous glucose monitoring vs. standard care in type 2 diabetes
- Physical activity interventions in patients with type 2 diabetes
- Dietary interventions for patients with type 2 diabetes
- Home blood pressure monitoring in hypertensive patients
- Telehealth interventions for hypertension management
- Nurse-led education programs for hypertension control
- Medication adherence programs for hypertensive patients
- Risk reduction strategies in patients with hyperlipidemia
- Patient education on insulin administration for type 1 diabetes
2. Cardiovascular Care
- Early mobilization in post-myocardial infarction patients
- Cardiac rehabilitation programs for heart failure patients
- Telemonitoring for congestive heart failure management
- Nurse-led blood pressure counseling in outpatient clinics
- Omega-3 supplementation in patients with coronary artery disease
- Home vs. hospital cardiac monitoring programs
- Stress reduction interventions for patients with high blood pressure
- Smoking cessation programs in cardiac patients
- Effectiveness of exercise interventions on cardiac output
- Patient education on heart failure symptom recognition
3. Critical Care & ICU
- Oxygen therapy vs. usual care in mechanically ventilated patients
- Prone positioning vs. standard care in ARDS patients
- Music therapy vs. no intervention for ICU anxiety
- Early mobilization vs. usual care in ICU patients
- Sedation protocols vs. standard care in mechanically ventilated patients
- Family-centered care vs. usual ICU routines
- Oral care interventions for ventilator-associated pneumonia prevention
- Delirium prevention protocols vs. standard ICU care
- Skin-to-skin care for premature infants in the NICU
- Noise reduction interventions for ICU patient comfort
4. Pain Management
- Music therapy vs. placebo in postoperative pain relief
- Guided imagery vs. usual care for chronic pain patients
- Acupuncture vs. standard analgesics in musculoskeletal pain
- Aromatherapy vs. placebo for postoperative pain
- Cognitive behavioral therapy vs. standard care for chronic pain
- Patient education on pain management vs. usual instructions
- Distraction techniques vs. standard care in pediatric pain management
- Heat therapy vs. cold therapy for musculoskeletal pain
- Massage therapy vs. usual care for post-surgical pain
- Psychological interventions vs. no intervention in pain reduction
5. Maternal and Neonatal Health
- Kangaroo care vs. incubator care for premature infants
- Early breastfeeding vs. delayed breastfeeding in neonatal weight gain
- Pain relief interventions vs. standard care during labor
- Continuous fetal monitoring vs. intermittent monitoring in high-risk pregnancies
- Home vs. hospital blood pressure monitoring for preeclampsia
- Skin-to-skin contact vs. usual care in postpartum bonding
- Maternal education on breastfeeding vs. standard instructions
- Exercise programs vs. usual care in postpartum recovery
- Iron supplementation adherence interventions in pregnant women
- Patient education on gestational diabetes management vs. standard care
6. Oncology
- Psychological interventions vs. no intervention in breast cancer patients
- Pain management education vs. usual care in cancer patients
- Physical activity vs. usual care in colorectal cancer patients
- Music therapy vs. placebo in reducing chemotherapy anxiety
- Cognitive behavioral therapy vs. standard care in cancer-related fatigue
- Nutritional counseling vs. standard diet advice in cancer patients
- Skin care interventions vs. usual care for radiation dermatitis
- Exercise interventions vs. standard care in breast cancer survivorship
- Telehealth follow-up vs. in-person visits for cancer patients
- Pain relief education programs vs. usual care in terminally ill patients
7. Respiratory Health
- Oxygen therapy vs. usual care in COPD patients
- Pulmonary rehabilitation vs. standard care in COPD patients
- Early mobilization vs. usual care in pneumonia patients
- Nebulizer therapy vs. inhaler therapy in asthma management
- Patient education on inhaler technique vs. standard instruction
- Home oxygen therapy vs. hospital monitoring in COPD patients
- Music therapy vs. no intervention in ventilated patients
- Telehealth monitoring vs. standard care in chronic respiratory patients
- Smoking cessation programs vs. usual care in COPD patients
- Incentive spirometry vs. usual care in post-surgical respiratory care
8. Infectious Diseases & Prevention
- Hand hygiene education vs. standard protocols for infection reduction
- Vaccination reminders vs. standard care for flu prevention
- Antibiotic stewardship programs vs. usual care in hospitals
- Patient education on wound care vs. standard instructions
- Early screening interventions vs. standard care in HIV patients
- Patient adherence interventions vs. usual care in TB management
- Mask usage education vs. no intervention in respiratory infections
- Nurse-led education on infection control vs. standard care
- Isolation protocols vs. standard care in hospital infection prevention
- Telehealth counseling vs. usual care for STI prevention
9. Mental Health
- Cognitive behavioral therapy vs. standard care for depression
- Mindfulness meditation vs. no intervention for anxiety
- Psychoeducation vs. standard care in schizophrenia management
- Music therapy vs. usual care for stress reduction
- Art therapy vs. placebo in mental health rehabilitation
- Teletherapy vs. in-person therapy for mood disorders
- Exercise interventions vs. usual care in depression management
- Patient education on coping strategies vs. standard instructions
- Peer support programs vs. no intervention in mental health recovery
- Psychological interventions vs. standard care for PTSD
10. Surgical Care & Postoperative Recovery
- Early mobilization vs. usual care in postoperative patients
- Pain management education vs. standard care
- Music therapy vs. placebo in post-surgical anxiety reduction
- Ice therapy vs. heat therapy for postoperative swelling
- Nutrition interventions vs. standard diet advice post-surgery
- Telemonitoring vs. in-person follow-up for surgical patients
- Pressure ulcer prevention vs. usual care in immobile post-op patients
- Patient education on wound care vs. standard instructions
- Nurse-led discharge education vs. usual care
- Early ambulation vs. standard care in abdominal surgery
11. Pediatrics
- Distraction therapy vs. usual care for procedural pain
- Education on asthma management vs. standard care
- Music therapy vs. no intervention for hospitalized children
- Parent-led kangaroo care vs. usual care in NICU
- Physical therapy vs. usual care for children with cerebral palsy
- Cognitive behavioral interventions vs. standard care in ADHD
- Telehealth interventions vs. in-person follow-up for pediatric diabetes
- Nutrition education vs. usual care for obese children
- Vaccination reminders vs. standard care in pediatric clinics
- Hand hygiene programs vs. usual care in pediatric wards
12. Geriatrics & Elderly Care
- Fall prevention programs vs. usual care in elderly patients
- Exercise interventions vs. usual care for elderly patients with osteoporosis
- Music therapy vs. placebo in pain reduction for elderly patients
- Cognitive stimulation vs. standard care for dementia patients
- Pressure ulcer prevention vs. usual care in immobile elderly patients
- Nutrition interventions vs. usual care in malnourished elderly
- Telehealth monitoring vs. usual care in elderly patients with chronic disease
- Medication adherence programs vs. standard care for elderly patients
- Social engagement programs vs. usual care for elderly in long-term care
- Pain management education vs. standard care in elderly patients
13. Lifestyle & Preventive Care
- Physical activity programs vs. usual care in obese patients
- Dietary counseling vs. standard advice for diabetes prevention
- Smoking cessation interventions vs. standard care
- Weight management programs vs. usual care in hypertensive patients
- Telehealth lifestyle coaching vs. standard care
- Stress reduction interventions vs. no intervention in high-risk patients
- Patient education on alcohol reduction vs. standard care
- Exercise adherence programs vs. usual care in cardiac patients
- Community health education vs. usual care for diabetes prevention
- Risk reduction counseling vs. standard care in cardiovascular patients
14. Special Interventions
- Negative pressure wound therapy vs. standard dressing care
- Skin-to-skin contact vs. usual care for premature infants
- Music therapy vs. placebo in mechanically ventilated patients
- Psychological interventions vs. no intervention for chronic pain
- Oxygen therapy protocols vs. standard care in ICU patients
- Telehealth vs. in-person interventions for chronic disease management
- Home care education vs. usual care for post-discharge patients
- Patient education on self-catheterization vs. standard instructions
- Pain relief interventions vs. standard care in burn patients
- Cognitive stimulation therapy vs. usual care in elderly patients
15. Quality of Life & Functional Outcomes
- Exercise interventions vs. usual care for stroke rehabilitation
- Occupational therapy vs. standard care for functional recovery
- Pain management programs vs. usual care in chronic pain patients
- Tele-rehabilitation vs. in-person therapy for mobility recovery
- Nutrition counseling vs. standard care for functional improvement
- Social support interventions vs. usual care for mental health outcomes
- Cognitive behavioral therapy vs. no intervention in chronic illness
- Patient education vs. usual care in improving adherence and quality of life
- Music therapy vs. placebo for anxiety reduction in hospitalized patients
- Early mobilization vs. usual care for improved recovery outcomes
What is a PICOT and how does the PICOT framework shape a research question?
A PICOT is a structured approach used to develop a clear and answerable research question within clinical research and nursing research. The term PICOT represents five core elements: the patient population, the intervention being considered, the comparison intervention or condition, the outcome of interest, and the time frame over which the outcome is measured. By organizing a research question into these components, the PICOT framework transforms a broad clinical concern into a focused and measurable inquiry.
In clinical settings, questions often emerge from observations in patient care, such as variations in outcomes, uncertainty about the effectiveness of a nursing intervention, or differences between usual care and alternative approaches. Without structure, these questions remain vague and difficult to investigate. The PICOT framework provides clarity by requiring that each element of the research question be explicitly defined. This ensures that the resulting research question aligns with relevant evidence and can guide the search for research evidence in a systematic way.
For example, instead of asking whether a particular intervention improves outcomes, a PICOT-based approach specifies which patients, which intervention, compared to what, and which health outcomes are being examined. This structured approach strengthens the research process and improves the precision of a nursing paper or research paper by ensuring that the question is neither too broad nor too narrow.
What is a picot question and how does it differ from a background question?
A PICOT question is a type of focused question designed to guide evidence-based inquiry and support the development of a research question suitable for systematic investigation. It differs fundamentally from a background question, which is typically broader and seeks general information rather than specific evidence.
A background question often addresses foundational knowledge, such as definitions, causes, or general characteristics of a condition. For instance, asking about the causes of hypertension or the general management of chronic obstructive pulmonary disease reflects a background question. While such questions are useful for building foundational understanding, they do not directly support clinical decision-making or intervention evaluation.
In contrast, a PICOT question narrows the focus to a specific clinical scenario. It asks whether a defined intervention leads to a measurable outcome when compared to standard care, usual care, or no intervention within a particular population. This distinction is critical in evidence-based nursing because PICOT questions are designed to identify relevant evidence that can inform practice decisions. A good PICOT question moves beyond general knowledge and directly addresses the result of the intervention in a way that can be tested through clinical research.
How does the pico framework help form a focused clinical question for nursing practice?
The PICO framework is a closely related model that includes four components: patient population, intervention, comparison, and outcome. While it does not explicitly include a time element, it remains highly effective for developing a focused clinical question in nursing practice. The PICO framework emphasizes clarity and relevance, ensuring that the question aligns with real-world clinical concerns and supports decision-making.
By requiring a clear definition of each component, the PICO framework prevents ambiguity in the formulation of a clinical question. For example, when examining pain management strategies, specifying whether the comparison is placebo, compared to no intervention, or compared to usual care ensures that the research question is precise and interpretable. This clarity is essential when evaluating interventions such as music therapy, psychological intervention, or oxygen therapy in specific patient populations.
The PICO framework also supports the identification of relevant evidence by aligning the clinical question with how studies are designed and reported in the literature. This alignment enhances the efficiency of literature searches and improves the quality of conclusions drawn from research findings. As a result, PICO questions that align with nursing practice are more likely to produce actionable insights that can improve patient care and inform healthcare providers.
Why is evidence-based practice important when developing a nursing picot question?
Evidence-based practice is central to the development of a nursing PICOT question because it ensures that clinical decisions are grounded in the best available evidence rather than tradition, assumption, or anecdotal experience. Evidence-based practice integrates research evidence, clinical expertise, and patient values to guide care decisions and improve health outcomes.
When developing a nursing PICOT question, evidence-based practice helps determine whether the proposed intervention is appropriate, measurable, and supported by existing research. It encourages the comparison of interventions to standard care, usual care, or placebo, allowing for objective evaluation of effectiveness. This approach is particularly important in areas such as chronic disease management, maternal health, critical care, and preventive interventions, where outcomes like incidence, blood pressure monitoring, blood glucose control, or oxygen saturation have direct clinical implications.
A PICOT question grounded in evidence-based practice also supports accountability in clinical research and nursing research. It ensures that the question aligns with ethical standards, clinical relevance, and feasibility, while also contributing to evidence-based nursing practice. By focusing on relevant evidence, the PICOT framework strengthens the link between research and nursing practice, ultimately supporting informed decision-making and improved patient outcomes.
How do nursing students choose a good PICOT topic for nursing research or a research paper?
Selecting an appropriate PICOT topic is a critical early step in the research process, as it determines the clarity, feasibility, and relevance of the resulting research question. Effective PICOT topics often emerge from real clinical challenges observed in nursing practice, gaps identified in existing research evidence, or areas where patient care outcomes vary despite similar conditions. A well-chosen topic should align with clinical relevance, availability of relevant evidence, and the ability to measure outcomes objectively.
A strong PICOT topic is typically centered on a clearly defined patient population and a modifiable nursing intervention. Topics that compare an intervention to standard care, usual care, or no intervention are particularly well suited for evidence-based inquiry. For example, examining whether a structured physical activity program reduces blood pressure in patients with hypertension compared to usual care provides a clear basis for developing a focused research question. Such topics lend themselves to systematic investigation and support evidence-based nursing practice.
What makes a good picot question for nursing students working on a research paper?
A good PICOT question is specific, focused, and answerable through clinical research. It clearly identifies the patient population, intervention, comparison, and outcome, ensuring that the research question is neither overly broad nor too narrow. Precision is essential, as a vague question may lead to inconsistent findings or difficulty locating relevant evidence.
An effective PICOT question also demonstrates a direct link between the intervention and the intended health outcomes. For instance, a question examining whether skin-to-skin contact improves oxygen saturation in premature babies compared to standard care clearly defines both the intervention and the measurable outcome. This clarity supports the identification of relevant evidence and strengthens the overall quality of the nursing research.
In addition, a good PICOT question aligns with the principles of evidence-based practice by allowing for comparison between interventions and outcomes that are clinically meaningful. Questions that specify whether an intervention leads to improved pain relief, reduced incidence of complications, or shorter length of stay are more likely to contribute valuable insights to nursing practice and clinical research.
How to narrow a research topic into a focused picot question for nursing school?
Broad research topics often require refinement before they can be transformed into focused PICOT questions. Narrowing a topic begins by identifying the specific patient population affected by the clinical issue and the nursing intervention under consideration. This process involves moving from a general research topic to a focused clinical question that can guide the research process.
For example, a broad topic such as pain management in elderly patients can be narrowed by specifying the intervention and comparison. A refined PICOT question might explore whether music therapy compared to placebo reduces pain levels in elderly patients receiving postoperative care. By defining the comparison and outcome, the research question becomes focused and suitable for systematic investigation.
The narrowing process also involves evaluating feasibility, including the availability of research evidence and the practicality of measuring outcomes. Focused PICOT questions are easier to evaluate, refine, and align with research guides used in nursing school and clinical research settings.
Which nursing research topics (eg. type 1 diabetes, hypertension, breast cancer) work well with PICOT?
Certain nursing research topics are particularly well suited to the PICOT framework because they involve measurable outcomes and clearly defined interventions. Chronic conditions such as type 1 diabetes, hypertension, and breast cancer are frequently explored using PICOT due to their prevalence and the availability of extensive research evidence.
For example, a PICOT-based research question might examine whether early blood glucose monitoring reduces the incidence of complications compared to standard care in patients with type 1 diabetes. Similarly, topics related to hypertension may focus on whether home blood pressure monitoring improves blood pressure control compared to usual care. In oncology-related research, questions might explore whether psychological intervention improves quality of life outcomes in patients undergoing treatment for breast cancer.
These topics are effective because they support the development of focused questions that align with evidence-based nursing practice. They allow for comparison of interventions, measurement of health outcomes, and integration of relevant evidence into nursing practice. By selecting topics that naturally align with the PICOT framework, researchers can ensure that their questions are both clinically meaningful and methodologically sound.
What are practical PICOT question examples and intervention PICOT ideas for clinical practice?
Practical PICOT question examples are designed to address real-world clinical challenges by evaluating the effectiveness of a specific intervention in improving patient care outcomes. In clinical practice, these questions often arise from uncertainty about whether a nursing intervention produces better health outcomes when compared to usual care, standard care, or no intervention. The PICOT framework supports the development of such questions by ensuring that each element of the clinical question is clearly defined and aligned with evidence-based practice.
Intervention PICOT ideas are particularly valuable because they focus on actions that can be implemented, measured, and evaluated within healthcare settings. These questions guide clinical research by identifying whether a nursing intervention leads to a meaningful result of the intervention, such as improved pain relief, reduced length of stay, or better physiological indicators. Well-constructed PICOT question examples serve as a bridge between nursing research and evidence-based nursing practice by translating clinical concerns into researchable questions supported by relevant evidence.
Which intervention picot examples compare music therapy versus placebo for pain management in elderly patients?
Pain management is a common focus of intervention PICOT questions, especially in populations where pharmacological approaches may present additional risks. Music therapy has been explored as a psychological intervention aimed at reducing pain perception and improving comfort. When framed using the PICOT framework, such questions allow for systematic evaluation of its effectiveness compared to placebo or no intervention.
An example of an intervention PICOT question in this context may examine whether music therapy compared to placebo results in improved pain relief among elderly patients experiencing postoperative pain. In this case, the intervention is clearly defined, the comparison establishes a control condition, and the outcome is measurable. This structure supports evidence-based nursing by enabling healthcare professionals to assess whether non-pharmacological approaches contribute to improved patient care.
By comparing music therapy to placebo, the question accounts for psychological factors that may influence pain perception, ensuring that the result of the intervention can be attributed to the intervention itself rather than external variables. Such PICOT question examples are particularly useful in clinical research focused on patient-centered care and non-invasive interventions.
How to frame a picot question for mechanically ventilated patients: oxygen therapy compared to usual care?
Mechanically ventilated patients in critical care environments present complex clinical challenges that require precise and evidence-based decision-making. Framing a PICOT question in this context involves clearly defining the patient population, the intervention, and the comparison to usual care. Oxygen therapy is frequently examined as an intervention aimed at improving oxygen saturation and overall health outcomes.
A focused PICOT question may explore whether a specific oxygen therapy protocol improves oxygen saturation compared to usual care in mechanically ventilated patients. By specifying the comparison to usual care, the question establishes a clear benchmark against which the intervention can be evaluated. This approach ensures that the research question aligns with clinical research standards and supports the identification of relevant evidence.
Such questions are essential in intensive care settings, including the ICU, where small changes in intervention protocols can significantly affect patient outcomes. By using the PICOT framework, healthcare providers can systematically assess whether modifications to oxygen therapy contribute to improved patient care and reduced complications.
Example PICOT: Does early blood glucose monitoring reduce incidence of complications compared to standard care in patients with type 1 diabetes?
Chronic disease management provides a strong foundation for PICOT question development due to the availability of measurable outcomes and established standards of care. In patients with type 1 diabetes, blood glucose control is a critical factor influencing the incidence of both short-term and long-term complications. Early blood glucose monitoring is a nursing intervention that can be evaluated using the PICOT framework.
A well-framed PICOT question in this context examines whether early blood glucose monitoring reduces the incidence of complications compared to standard care in patients with type 1 diabetes. This question clearly defines the patient population, intervention, comparison, and outcome, making it suitable for evidence-based practice and clinical research. The outcome, incidence of complications, is measurable and clinically meaningful, supporting the evaluation of the intervention’s effectiveness.
This type of PICOT question highlights how structured clinical inquiry can guide nursing research and improve patient care. By comparing early monitoring to standard care, the question supports objective assessment and contributes to evidence-based nursing practice focused on improving health outcomes through targeted nursing intervent
How do you write a good PICOT question for evidence-based nursing and research process?
Writing a good PICOT question is a structured exercise that aligns clinical inquiry with evidence-based nursing and the broader research process. A well-constructed PICOT question begins with a clearly identified clinical question that arises from nursing practice, patient care challenges, or gaps in current research evidence. The purpose of the PICOT framework is to transform this initial inquiry into a focused question that can guide literature searches, data collection, and evaluation of health outcomes.
A good PICOT question demonstrates clarity, relevance, and feasibility. Each component—patient population, intervention, comparison, and outcome—must be explicitly defined to avoid ambiguity. For example, rather than asking whether an intervention improves outcomes, a focused PICOT question specifies whether a nursing intervention improves a measurable outcome when compared to standard care or usual care. This precision ensures that the question aligns with evidence-based practice and can be addressed using existing clinical research.
Importantly, a good PICOT question supports evidence-based nursing practice by facilitating the identification of relevant evidence and enabling objective evaluation of the result of the intervention. Questions that are structured using PICOT are more likely to lead to meaningful conclusions that inform clinical decision-making and improve patient care.
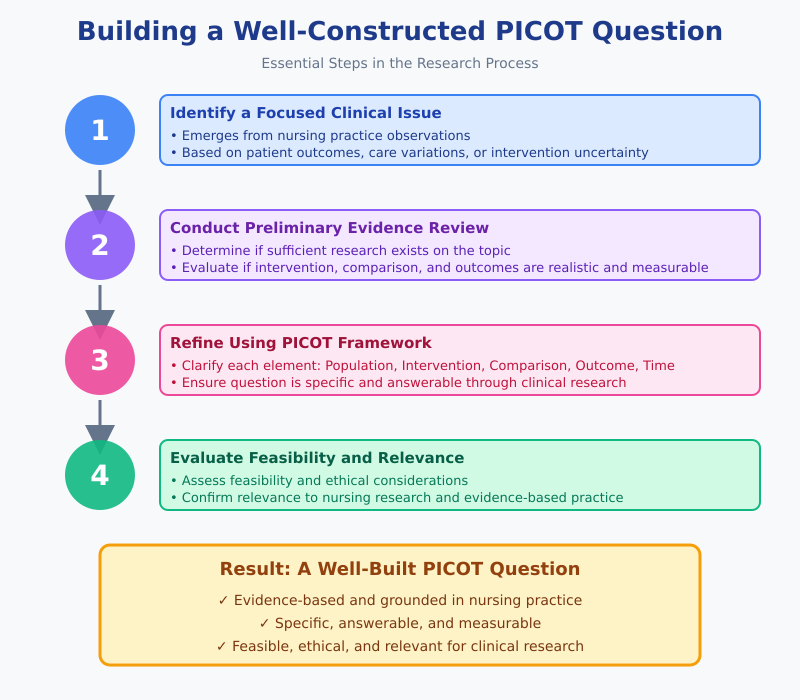
What steps in the research process ensure a well-built picot question for evidence-based nursing?
The development of a strong PICOT question is closely tied to the steps of the research process. The first step involves identifying a focused clinical issue grounded in nursing practice. This issue often emerges from observations related to patient outcomes, variations in care, or uncertainty about the effectiveness of an intervention.
The next step is conducting a preliminary review of relevant evidence to determine whether sufficient research exists on the topic. This step helps refine the research question and ensures alignment with evidence-based practice. During this stage, the researcher evaluates whether the intervention, comparison, and outcomes are realistic and measurable.
Refinement of the research question follows, using the PICOT framework to clarify each element. This step ensures that the research question is specific and answerable through clinical research. Finally, the question is evaluated for feasibility, ethical considerations, and relevance to nursing research. These steps collectively ensure that the PICOT question is well built, evidence based, and suitable for inclusion in a nursing paper or research paper.
How to convert a clinical question into a picot question: PICO question templates and tips?
Converting a clinical question into a PICOT question involves moving from a general inquiry to a focused question that can guide systematic investigation. A clinical question often begins broadly, such as whether a particular intervention improves patient outcomes. Using the PICO framework, this question is refined by clearly identifying the patient population, intervention, comparison, and outcome.
PICO question templates are useful tools in this conversion process. A common template follows this structure: In [patient population], how does [intervention] compared to [comparison] affect [outcome]? This format ensures that the question remains focused and aligned with clinical research standards.
For example, a general clinical question about pain management can be converted into a PICOT question by specifying whether a psychological intervention improves pain relief compared with no intervention in a defined population. This structured approach enhances clarity and supports the identification of relevant evidence. Using such templates ensures that the resulting PICOT question aligns with evidence-based nursing practice and contributes meaningfully to the research process.
When should nursing students use evidence-based practice and compared to no intervention designs in PICOT?
Evidence-based practice should guide the selection of comparison groups in PICOT questions, including decisions about when to use compared to no intervention designs. Such designs are appropriate when evaluating whether an intervention provides measurable benefits beyond the absence of active treatment or usual care. This approach is particularly useful when assessing non-invasive or supportive interventions where withholding treatment does not pose ethical concerns.
Compared to no intervention designs allow researchers to isolate the effect of the intervention and determine whether observed changes in health outcomes can be attributed directly to the nursing intervention. For instance, evaluating whether music therapy improves pain relief compared with no intervention provides insight into the effectiveness of the intervention itself. These designs are commonly used in evidence-based nursing and clinical research to establish baseline effectiveness.
The choice to use a no-intervention comparison must always consider ethical standards, patient safety, and the availability of existing standard care. When applied appropriately, such designs strengthen the validity of the PICOT question and support the generation of high-quality research evidence that informs nursing practice and healthcare decision-making.
What PICOT examples address specific patient populations like premature babies, pregnant women, or ICU patients?
Developing effective PICOT questions requires careful consideration of the patient population, intervention, comparison, outcomes, and sometimes time frame. Comprehensive examples demonstrate how these elements interact to produce researchable, actionable questions that inform evidence-based nursing practice. The examples below illustrate PICOT questions across a variety of clinical settings and interventions.
What is a strong nursing picot question for premature babies: kangaroo care compared to usual care?
Premature Babies – Kangaroo Care
Clinical Scenario: Premature infants in neonatal intensive care are at high risk for complications related to immature physiological systems. Skin-to-skin contact (kangaroo care) has been proposed as a nursing intervention to improve outcomes.
PICOT Question:
In premature babies (P), does kangaroo care (I) compared to usual incubator care (C) improve oxygen saturation levels and reduce the length of hospital stay (O) within the first two weeks of life (T)?
Explanation:
- Population: Premature babies
- Intervention: Kangaroo care (skin-to-skin contact)
- Comparison: Usual incubator care
- Outcome: Improved oxygen saturation and reduced length of stay
- Time: First two weeks of life
This question is comprehensive because it identifies measurable physiological outcomes, a clear intervention, and a practical comparison, making it suitable for both clinical research and evidence-based nursing practice.
How to develop a picot question for pregnant women: pain relief or blood pressure monitoring interventions?
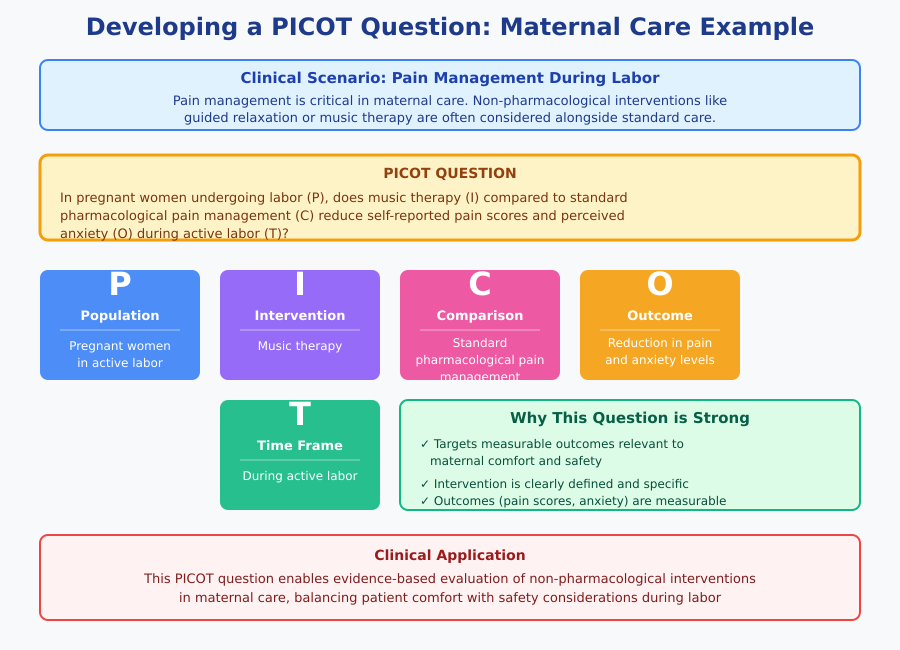
Pregnant Women – Pain Relief During Labor
Clinical Scenario: Pain management during labor is a critical aspect of maternal care. Non-pharmacological interventions, such as guided relaxation or music therapy, are often considered alongside standard care.
PICOT Question:
In pregnant women undergoing labor (P), does music therapy (I) compared to standard pharmacological pain management (C) reduce self-reported pain scores and perceived anxiety (O) during active labor (T)?
Explanation:
- Population: Pregnant women in active labor
- Intervention: Music therapy
- Comparison: Standard pharmacological pain management
- Outcome: Reduction in pain and anxiety levels
- Time: During active labor
This question is strong because it targets measurable outcomes relevant to maternal comfort and safety, and the intervention is clearly defined.
Which research questions suit ICU or mechanically ventilated patients focused on oxygen therapy or music therapy?
ICU or Mechanically Ventilated Patients – Oxygen Therapy
Clinical Scenario: Mechanically ventilated patients require optimal oxygen delivery to maintain physiological stability. Adjusting oxygen therapy protocols may improve outcomes.
PICOT Question:
In mechanically ventilated ICU patients (P), does titrated oxygen therapy to maintain target oxygen saturation levels (I) compared to standard oxygen therapy (C) reduce incidence of hypoxemia and length of ICU stay (O) over a one-week period (T)?
Explanation:
- Population: Mechanically ventilated ICU patients
- Intervention: Titrated oxygen therapy
- Comparison: Standard oxygen therapy
- Outcome: Reduced incidence of hypoxemia and length of ICU stay
- Time: One week
This question is comprehensive because it considers clinically relevant physiological outcomes, a defined intervention, and an appropriate comparison, ensuring applicability in evidence-based nursing practice.
Type 1 Diabetes – Early Blood Glucose Monitoring
Clinical Scenario: Early intervention in patients with type 1 diabetes can prevent complications and improve long-term outcomes.
PICOT Question:
In patients with type 1 diabetes (P), does early and frequent blood glucose monitoring (I) compared to standard monitoring protocols (C) reduce the incidence of hypoglycemia, hyperglycemia, and hospital admissions (O) over a six-month period (T)?
Explanation:
- Population: Patients with type 1 diabetes
- Intervention: Early and frequent blood glucose monitoring
- Comparison: Standard monitoring
- Outcome: Reduced incidence of glucose fluctuations and hospital admissions
- Time: Six months
This question is highly practical for clinical research and demonstrates a clear connection between intervention, outcomes, and evidence-based nursing practice.
Elderly Patients – Music Therapy for Pain Management
Clinical Scenario: Elderly patients in postoperative care often experience pain that may not be fully managed by pharmacological interventions.
PICOT Question:
In elderly patients recovering from surgery (P), does music therapy (I) compared to placebo (C) reduce pain scores and opioid consumption (O) during the first 48 hours postoperatively (T)?
Explanation:
- Population: Elderly postoperative patients
- Intervention: Music therapy
- Comparison: Placebo
- Outcome: Reduced pain scores and opioid use
- Time: First 48 hours postoperatively
This question illustrates a practical, evidence-based intervention that can be tested and measured, and the outcomes directly impact patient care and resource utilization.
Key Considerations for Comprehensive PICOT Questions
- Clarity and Specificity: Each component of the PICOT framework should be defined explicitly.
- Measurable Outcomes: The outcome must be quantifiable, such as blood pressure, oxygen saturation, length of stay, or incidence of complications.
- Relevance to Evidence-Based Practice: The intervention should have a clear rationale and be supported by existing research or clinical guidelines.
- Feasibility: Consider available resources, ethical considerations, and patient safety when selecting interventions and outcomes.
How to evaluate and refine PICOT question examples for evidence-based practice and clinical research?
Evaluating and refining PICOT questions is an essential step in ensuring that research questions are both clinically relevant and methodologically sound. A well-evaluated PICOT question aligns with evidence-based nursing and the goals of clinical research by clearly defining the patient population, intervention, comparison, outcome, and time frame. Refinement begins with a critical review of the question’s clarity, specificity, and feasibility.
For example, a PICOT question such as, “Does early blood glucose monitoring improve outcomes in patients with type 1 diabetes?” may initially appear broad. Refinement involves specifying measurable outcomes, comparison groups, and time frames: “In patients with type 1 diabetes (P), does early blood glucose monitoring (I) compared to standard monitoring protocols (C) reduce the incidence of hypoglycemia and hospital admissions (O) over six months (T)?” This refinement makes the question actionable, measurable, and aligned with clinical practice.
Additional strategies for refinement include:
- Ensuring the intervention and comparison are feasible within the clinical setting.
- Confirming that outcomes are measurable and clinically meaningful.
- Checking alignment with current evidence-based practice guidelines.
- Reviewing existing literature to ensure the question addresses a knowledge gap.
How to test if a picot question is feasible and evidence-based for a research project?
Feasibility is a critical consideration when developing PICOT questions. A feasible question is one that can realistically be studied within available resources, time constraints, and ethical parameters. Feasibility testing involves evaluating whether:
- The patient population is accessible.
- The intervention can be applied safely and ethically.
- Outcomes are measurable with available tools and techniques.
- Data collection methods are practical and reliable.
For instance, a PICOT question evaluating oxygen therapy in mechanically ventilated patients is feasible if the ICU has sufficient equipment to implement the intervention and monitor outcomes like oxygen saturation and length of stay.
Evidence-based evaluation involves reviewing the literature to determine whether the intervention has been previously studied and whether there is sufficient high-quality evidence to support the question. This step ensures that the research is grounded in relevant evidence and aligns with evidence-based nursing practice. Systematic reviews, clinical guidelines, and peer-reviewed studies are reliable sources for evaluating whether the PICOT question is supported by existing research.
What criteria define a good picot question when comparing interventions to standard care or no intervention?
A good PICOT question comparing interventions to standard care or no intervention demonstrates several key characteristics:
- Clarity: Each element of PICOT is explicitly defined. For example, “In elderly postoperative patients (P), does music therapy (I) compared to placebo (C) reduce pain scores (O) during the first 48 hours postoperatively (T)?”
- Measurability: Outcomes should be objective and quantifiable, such as blood sugar levels, blood pressure readings, or pain scores.
- Clinical Relevance: The intervention should have the potential to improve patient care outcomes in a meaningful way.
- Ethical Considerations: Comparison to no intervention should be ethically acceptable, ensuring patients are not deprived of essential care.
- Alignment with Evidence-Based Practice: The question should build on existing research or fill an identified knowledge gap.
By meeting these criteria, PICOT questions allow for structured, ethical, and meaningful comparisons between interventions and standard care or no intervention, facilitating the generation of actionable evidence for clinical practice.
How to link picot question outcomes to health outcomes like blood sugar levels, pain relief, or risk of developing complications?
Linking PICOT question outcomes to health outcomes ensures that research findings are clinically meaningful and applicable to patient care. To achieve this, it is essential to:
- Define measurable indicators for each outcome: For example, blood sugar levels can be measured as fasting plasma glucose or HbA1c levels; pain relief can be assessed using a standardized pain scale; and risk of developing complications can be quantified as incidence rates.
- Ensure temporal relevance: Include a time frame that allows for measurable changes in outcomes, such as monitoring blood glucose over six months or assessing pain scores during the first 48 hours postoperatively.
- Select outcomes that reflect patient-centered care: Focus on results that directly affect patient safety, recovery, or quality of life, such as reduced hospital admissions, improved oxygen saturation, or decreased incidence of pressure ulcers.
- Align outcomes with the intervention and comparison: Outcomes must logically connect to the nursing intervention and the control or comparison group to provide meaningful evidence about effectiveness.
For example, a comprehensive PICOT question might be:
“In patients with hypertension (P), does home blood pressure monitoring (I) compared to standard clinic monitoring (C) reduce blood pressure levels (O) and the risk of cardiovascular complications (O) over a 12-week period (T)?”
Here, the outcomes—blood pressure levels and risk of cardiovascular complications—are directly measurable, clinically significant, and linked to the intervention, making the PICOT question robust, evidence-based, and aligned with patient care goals.
Conclusion
The PICOT framework serves as a cornerstone for developing structured, focused, and clinically relevant research questions in nursing practice. By systematically defining the patient population, intervention, comparison, outcome, and time frame, PICOT questions transform broad clinical concerns into measurable, evidence-based inquiries that directly inform patient care. Well-constructed PICOT questions not only guide the research process but also enhance the rigor, clarity, and relevance of nursing research papers, ensuring that interventions are evaluated scientifically and applied effectively in real-world settings.
Selecting a good PICOT topic begins with identifying gaps in clinical practice, areas of uncertainty, or populations at risk for adverse outcomes. Refining these topics into focused PICOT questions requires careful consideration of feasibility, ethical standards, and alignment with evidence-based nursing. Practical examples—ranging from blood glucose monitoring in patients with type 1 diabetes to music therapy for pain relief in elderly or mechanically ventilated patients—illustrate how the framework bridges research with meaningful health outcomes, including improved pain management, reduced complications, and enhanced quality of life.
Moreover, the PICOT framework supports the integration of evidence-based practice into daily nursing care, ensuring that interventions are not only theoretically sound but also demonstrably effective. By linking research questions to measurable outcomes, nurses and healthcare providers can make informed decisions that optimize patient safety, promote recovery, and strengthen overall healthcare delivery.
Ultimately, mastering the art of crafting comprehensive PICOT questions equips nurses and researchers with a powerful tool to advance clinical knowledge, implement targeted interventions, and contribute to a culture of continuous improvement in nursing practice. The framework’s emphasis on clarity, specificity, and evidence-based reasoning ensures that each question is not merely an academic exercise, but a meaningful step toward improving health outcomes across diverse patient populations.
Frequently Asked Questions
What are some good research topics for nursing students?
Good research topics often focus on improving patient care, addressing gaps in clinical practice, or evaluating interventions. Examples include:
- Blood glucose monitoring and management in type 1 or type 2 diabetes
- Pain management strategies in elderly or postoperative patients
- Music therapy or psychological interventions for ICU patients
- Prevention of pressure ulcers in immobile patients
- Telehealth interventions for chronic disease management
What are some hot topics in nursing?
Current trending areas in nursing research and practice include:
- Evidence-based interventions for chronic disease management
- Telehealth and remote patient monitoring
- Nurse-led programs for mental health support
- Patient safety and infection prevention
- Palliative care and end-of-life interventions
- Innovations in ICU care and mechanically ventilated patient management
What are some hot topics in nursing?
Current trending areas in nursing research and practice include:
- Evidence-based interventions for chronic disease management
- Telehealth and remote patient monitoring
- Nurse-led programs for mental health support
- Patient safety and infection prevention
- Palliative care and end-of-life interventions
- Innovations in ICU care and mechanically ventilated patient management
What are some examples of evidence-based practice in nursing?
Evidence-based practice integrates clinical expertise with the best available research. Examples include:
- Using skin-to-skin contact (kangaroo care) to improve outcomes for premature babies
- Implementing early mobilization protocols in ICU patients
- Music therapy for pain and anxiety relief in elderly or post-surgical patients
- Home blood pressure monitoring programs for hypertension management
- Telehealth-based diabetes education and monitoring
