Controversial Medical Healthcare Topics: Ethical Issues and Medical Controversies Facing Healthcare Providers in 2026
Controversial medical healthcare topics are an integral part of understanding the complexities of modern medical practice and patient care. Just as evidence-based guidelines inform clinical decision-making, exploring medical controversies equips nursing students with the critical thinking skills needed to navigate ethical dilemmas and complex situations in healthcare settings. Far from being theoretical discussions, these topics—ranging from reproductive health and long-term care to digital health and behavioral health—directly influence patient outcomes, healthcare delivery, and the responsibilities of healthcare providers.
At the heart of these discussions are ethical issues and medical ethics, which provide a framework for evaluating professional responsibilities, patient rights, and systemic challenges. By studying controversial medical topics, nursing students gain insight into how issues in healthcare can shape policies, affect access to care, and impact health equity within diverse populations. Understanding these debates also highlights the implications of healthcare costs, Medicare policies, and resource allocation, emphasizing the real-world consequences of clinical and administrative decisions.
This guide offers a comprehensive examination of key controversies facing healthcare in 2024 and beyond, illustrating how these debates intersect with patient care, medical practice, and the evolving health system. Examples from recent cases and contemporary discussions will illuminate both the challenges and opportunities nursing students may encounter in their professional development. By engaging with these topics, future nurses can cultivate informed perspectives, advocate for equitable healthcare services, and uphold ethical standards across clinical settings.
Ultimately, studying controversial medical healthcare topics is about more than knowledge acquisition—it is about preparing nursing students to respond thoughtfully, ethically, and effectively to the complex realities of patient care, while contributing to a healthcare system that values both excellence and equity.
What are the major medical controversies nursing students should study?
Nursing students must engage with major controversial medical issues because these debates shape the healthcare system they will work in and affect how healthcare providers make complex decisions. Some controversies have deep historical roots, while others have emerged more recently as science, society, and policy evolve.
One enduring area of debate is the appropriate use of electronic health records. Questions about interoperability, data access, and vendor market dominance have sparked industry‑wide scrutiny; for example, Epic Systems has faced antitrust lawsuits alleging that its health information systems limit competition and restrict patient data flows to competitors, raising concerns about access and market fairness.
Another long‑standing controversial medical topic is the allocation of limited clinical resources. Decisions about who receives certain treatments or how aggressively to pursue diagnostic interventions can fundamentally influence patient care and raise ethical questions about fairness and clinical benefit. Evidence debates about procedures once considered routine — like certain arthroscopic knee operations or elective cardiac interventions — highlight the tension between traditional practice and evidence‑based scrutiny.
Additionally, high‑impact areas like reproductive health remain fiercely debated. Access to medication abortion through telehealth has grown significantly in 2025 as patients seek alternatives in restrictive legal environments, illustrating how service delivery innovations intersect with policy and rights issues.
Emerging technologies such as digital health — including AI‑driven diagnostics, telemedicine, and mobile health solutions — are also at the forefront of controversy. While these tools promise better health outcomes and system efficiencies, they invite debates about algorithmic bias, equitable access, and clinical reliability.
Which controversial medical topics are most debated in the healthcare system?
Several issues in healthcare consistently dominate professional and public discussions:
1. Clinical Decision Tools and Technology
The rapid expansion of AI in diagnostics and administrative workflows illustrates both promise and concern. While predictive models can enhance early disease detection, questions remain about accountability when these systems err, especially in life‑critical scenarios. Such debates reflect broader concerns over digital transformation and reliance on automated decision support.
2. Access and Equity
Disparities in access to care continue to be hotly debated. Interventions that expand coverage (such as managed care models) may conflict with cost pressures and provider hesitancy, influencing who receives care and at what quality level.
3. Reproductive Rights and Service Delivery
The aftermath of landmark policy shifts — particularly related to abortion access — have spurred ongoing controversies about legal protections, telehealth service scope, and implications for related procedures such as IVF.
4. Healthcare Costs and Insurance Structures
Rising healthcare costs and debates over Medicare payment reforms illustrate how financing models can influence care decisions, practice viability, and patient affordability — realities that frontline nurses witness daily.
How do medical controversies affect patient care and medical practice?
Medical controversies have a direct impact on both what happens at the bedside and how the health system functions:
- Clinical Uncertainty: When evidence is conflicting — such as debates about the routine use of certain surgical procedures — clinicians and nurses must weigh patient preferences against best evidence, sometimes adjusting care plans in real time.
- Policy Shifts Affect Services: Legislative debates around telehealth reimbursements or service eligibility can expand or restrict how providers deliver care, especially for remote patients or those seeking behavioral health services.
- Trust and Communication: When controversies like AI use or reproductive care dominate headlines, patients may doubt clinical recommendations, leading to communication challenges and the need for enhanced patient education.
- Resource Allocation: Heated debates over Medicare payment rates or funding for community‑based programs can strain smaller practices, influence staffing models, and even affect patient access in underserved regions.
What recent 2026 examples highlight issues in healthcare and medical controversies?
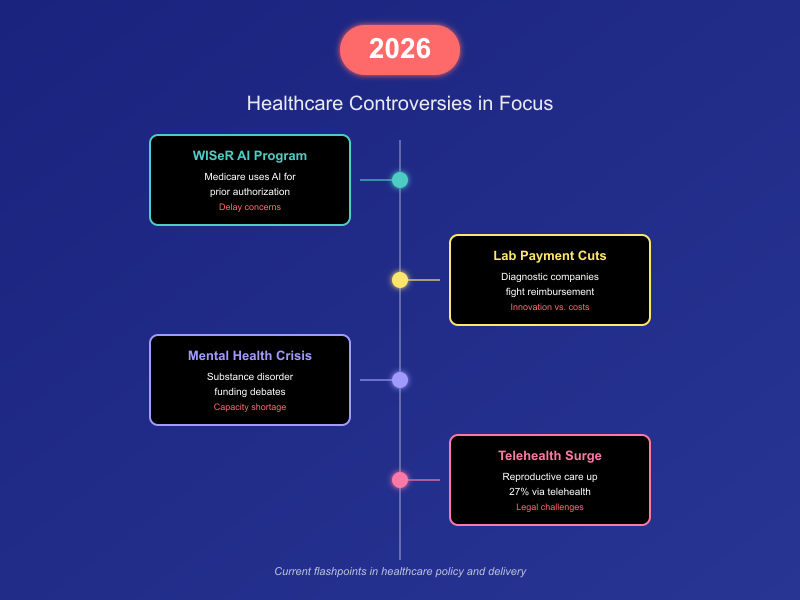
Several current events and policy debates in 2026 vividly illustrate how issues facing the health system continue to evolve:
1. AI and Prior Authorization
In 2026, a pilot Medicare program known as WISeR is deploying artificial intelligence to approve or deny medical procedures before service delivery. While proponents argue this could reduce waste, critics — including professional associations and some clinicians — express concern that algorithmic denial decisions could delay necessary treatments and undermine clinical judgment, illustrating real‑world controversy at the intersection of technology and patient care.
2. Medicare Payment Debates
Diagnostic lab companies are actively lobbying against significant Medicare reimbursement cuts scheduled for 2026. Their argument is that reduced payments could hinder investment in advanced testing technologies essential for patient safety and disease detection, creating tensions between cost containment and innovation.
3. Mental Health Policy Shifts
Recent policy proposals impacting funding and access to substance use disorder services reflect broader debates about system priorities, especially as behavioral health needs grow and service capacity lags behind demand.
4. Telehealth and Reproductive Care Access
The continued rise in telehealth‑based abortion services — up 27% in 2025 — underscores how evolving delivery methods challenge existing legal frameworks and surveillance policies, foreshadowing further debate as we move into 2026.
How do ethical issues and medical ethics shape clinical decision-making?
Ethical considerations are central to every clinical encounter. Ethical issues arise when providers must choose between competing values—for example, when a treatment with potential benefit carries significant risk, when patient wishes conflict with clinical recommendations, or when scarce resources require prioritization. At the core of medical ethics are principles such as autonomy (respecting a patient’s right to make decisions), beneficence (acting in the patient’s best interests), non‑maleficence (avoiding harm), and justice (fairness in distributing benefits and burdens). These principles are not abstract; they directly influence everyday judgments about diagnosis, treatment, and communication.
For example, consider a patient with advanced illness who refuses a recommended intervention. A nurse must balance respect for the individual’s preferences with professional assessment of what constitutes beneficial action. In such moments, ethical frameworks guide clinicians to honor autonomy while ensuring that the patient is fully informed. Decision‑making tools such as ethics consultations or institutional ethics committees can support clinical judgment, especially in high‑stakes situations where values conflict.
What are common medical ethical dilemmas encountered by healthcare providers?
Clinicians regularly face medical ethical dilemmas that test both personal and professional commitments. One common scenario involves patient confidentiality: When a patient reveals information that poses a risk to others (for example, an infectious disease that could spread), nurses and other staff must navigate legal obligations to report with commitments to privacy and trust. Another dilemma occurs when patients lack decision‑making capacity—such as in advanced dementia—requiring providers to work with surrogate decision‑makers while upholding the patient’s known or presumed wishes.
In emergency settings, the urgency of care can create tension between immediate action and informed consent. For instance, if a patient is unconscious and time‑sensitive care is required to prevent permanent harm, the principle of beneficence may justify intervention without explicit consent, but this must be balanced with respect for autonomy as soon as possible.
How should nursing students approach ethical issues in patient care?
Approaching ethical challenges requires a combination of knowledge, reflection, and collaboration. First, nursing students should become familiar with ethical standards articulated by professional organizations, such as the American Nurses Association Code of Ethics, which provides guidance on integrity, advocacy, and respect for human dignity. Students should practice structured critical thinking—identifying the facts of a situation, the values at stake, the stakeholders involved, and the potential consequences of different actions.
Communication skills are also vital. Engaging patients and families in open, compassionate dialogue helps clarify values and expectations, and improves shared understanding. Team communication is equally important; consulting with physicians, social workers, or ethics committees can broaden perspectives and strengthen decision‑making. Reflective practice—thinking about experiences after the fact—enables students to learn from ethical challenges and refine their judgment over time.
For example, when caring for a terminally ill patient weighing the benefits and burdens of continued aggressive treatment, a nursing student should ask: What are the patient’s goals? How might interventions affect their quality of care and daily experience? Are there psychosocial or spiritual concerns that need attention? Integrating these questions into care planning supports ethically sound decisions.
What role does medical ethics play in preventing medical errors?
Medical errors—events that could have been prevented and that may harm patients—are a significant concern in healthcare. Ethical practice plays a crucial role in both preventing and responding to these errors. A culture grounded in ethics emphasizes patient safety as a fundamental value and encourages reporting and transparency without fear of punishment. When clinicians are instructed to disclose errors honestly to patients and families, trust is preserved, and system weaknesses can be identified and corrected.
Ethical reflection also underpins the use of evidence‑based practices that reduce harm. For instance, standardized checklists for procedures such as central line insertion or surgical time‑outs have been shown to decrease complications. These practices reflect a commitment to non‑maleficence and beneficence by minimizing risk and enhancing outcomes.
Education on ethical obligations also fosters vigilance. Recognizing systemic factors that contribute to errors—such as fatigue, communication breakdowns, or inadequate staffing—enables clinicians to advocate for changes that protect patients. In this way, ethics is not merely a theoretical concern but a practical force that drives improvements in care processes and supports safer clinical environments.
What controversial topic in reproductive health should nurses be prepared to discuss?
1. Abortion and Pregnancy Termination
- Access to safe abortion services
- Legal status of abortion in different countries
- Telehealth abortion services
- Medication abortion versus surgical abortion
- Third-trimester abortion controversies
- Parental consent laws for minors
- Abortion and religious beliefs
- Abortion counseling and informed consent
- Abortion stigma and mental health
- Abortion access in rural areas
- Emergency contraception and abortion debates
- Abortion funding and insurance coverage
- Abortion restrictions and maternal health outcomes
- Unsafe abortion practices globally
- Abortion and conscientious objection by healthcare providers
- Role of nurses in post-abortion care
- Ethical debates around selective abortion
- Abortion and adolescent health rights
- Post-abortion contraception counseling
- Social determinants affecting abortion access
- Cultural perspectives on abortion
- Abortion and health equity
- Political influences on abortion policy
- Abortion and patient autonomy
- Abortion litigation and legal precedents
2. Contraception and Family Planning
- Access to birth control for minors
- Emergency contraception availability
- Long-acting reversible contraception (LARC) controversies
- Hormonal contraception and cardiovascular risks
- Contraception in religious institutions
- Contraceptive mandates under insurance policies
- Male contraception research and ethics
- Contraceptive education in schools
- Equity in access to contraceptive services
- Cultural attitudes toward contraception
- Contraception and adolescent pregnancy prevention
- Informed consent for contraceptive use
- Contraceptive failure and liability
- Contraception in low-income populations
- Reproductive coercion and ethical issues
- Contraceptive methods and weight gain debates
- Contraception and mental health outcomes
- Role of nurses in contraceptive counseling
- Digital health apps for family planning
- Contraception and privacy concerns
- Over-the-counter versus prescription contraception
- Government-funded contraceptive programs
- Emergency contraception and religious objections
- Access disparities between urban and rural areas
- Contraception and patient autonomy
3. Fertility and Assisted Reproductive Technology (ART)
- IVF and ethical considerations
- Surrogacy laws and regulations
- Egg and sperm donation ethics
- Genetic screening in ART
- Cost and access to fertility treatments
- Age limits for ART
- Single parent access to fertility services
- LGBTQ+ access to ART
- Ethical debates over embryo freezing
- Use of donor embryos
- ART success rates and patient counseling
- ART and multiple pregnancies risks
- Ethical considerations in preimplantation genetic testing
- Cross-border reproductive care
- Insurance coverage for fertility treatments
- Fertility preservation in cancer patients
- Egg sharing and compensation controversies
- ART and long-term child outcomes
- Ethical concerns around embryo disposal
- Role of nurses in ART counseling
- Reproductive tourism and regulatory issues
- Cultural attitudes toward fertility treatments
- ART access in low-resource settings
- Religious perspectives on ART
- Psychological impact of ART failure
4. Pregnancy and Maternal Health
- High-risk pregnancy management ethics
- Maternal mortality disparities
- Home birth versus hospital birth debates
- Cesarean section overuse
- VBAC (Vaginal Birth After Cesarean) controversies
- Pain management during labor
- Epidural use and informed consent
- Midwifery versus obstetrician-led care
- Birthing plans and patient autonomy
- Forced interventions in childbirth
- Maternal-fetal conflict in clinical decision-making
- Maternal age and pregnancy risks
- Pregnancy termination for maternal health
- Nutrition and maternal outcomes
- Substance use in pregnancy
- Gestational diabetes management ethics
- Hypertensive disorders in pregnancy
- Ethical issues in prenatal screening
- Prenatal care access disparities
- Maternal mental health and postpartum depression
- Assisted labor induction controversies
- Health system resource allocation in pregnancy care
- Fetal monitoring and labor management
- Cultural practices in pregnancy care
- Nurses’ role in advocating for maternal rights
5. Sexual Health and STIs
- STI screening ethics
- Confidentiality in adolescent sexual health
- HIV disclosure and legal issues
- PrEP access and equity
- HPV vaccination controversies
- Sexual health education in schools
- Condom access for minors
- Cultural attitudes toward sexual health
- Partner notification in STI management
- Testing without consent for minors
- STI prevention campaigns and effectiveness
- Ethical dilemmas in STI treatment
- Risk compensation and preventive measures
- Role of nurses in sexual health counseling
- Confidentiality in telehealth sexual health services
- STI stigma and patient adherence
- Resource allocation for STI prevention
- LGBTQ+ sexual health disparities
- Behavioral interventions in sexual health
- Consent issues in sexual health research
- Parental involvement in STI care
- Access to PrEP in rural populations
- Public health versus individual autonomy
- Ethical concerns with partner tracing
- Digital health platforms for sexual health
6. Reproductive Rights and Policy
- Roe v. Wade implications (U.S.)
- Access to reproductive health services globally
- Insurance coverage of reproductive care
- Conscientious objection by providers
- Government funding for reproductive health
- Equity in reproductive health policies
- Maternal leave policies and health outcomes
- Legal restrictions on abortion and contraception
- Reproductive health advocacy
- Patient education and informed consent policies
- Health policy impact on fertility treatments
- Reproductive justice frameworks
- Access disparities by socioeconomic status
- Digital health policy in reproductive care
- Global reproductive health goals
- Cross-border reproductive care regulations
- Ethical implications of reproductive legislation
- Nurses’ role in health policy advocacy
- Maternal health funding priorities
- Abortion pill access and policy debates
- Telehealth reproductive care regulations
- Policy-driven disparities in contraceptive access
- Mandatory counseling laws for abortion
- Ethical issues in government-mandated reproductive reporting
- Patient confidentiality in reproductive health data
7. Adolescent Reproductive Health
- Early sexual education and controversies
- Access to contraception for teenagers
- Parental consent requirements
- Confidentiality in adolescent care
- Teen pregnancy prevention programs
- Mental health support for teen pregnancies
- STI screening in minors
- Cultural barriers to adolescent reproductive health
- Peer education effectiveness
- School-based reproductive health services
- Ethical dilemmas in adolescent consent
- Telehealth services for teenagers
- Substance use and reproductive risk in adolescents
- LGBTQ+ adolescent reproductive health
- Adolescent fertility education
- Social media influence on adolescent health
- Adolescent access to abortion services
- Confidential counseling in schools
- Adolescent maternal health disparities
- Health literacy in reproductive topics
- Risk behaviors and intervention strategies
- Confidential reporting requirements
- Vaccination access and adolescent consent
- Ethical considerations in adolescent research
- Adolescents and reproductive health advocacy
8. Emerging and Controversial Reproductive Health Topics
- Fertility tracking apps and privacy concerns
- AI in reproductive health diagnostics
- Genetic editing and CRISPR in embryos
- Sex-selective abortion controversies
- Maternal surrogacy exploitation risks
- Reproductive technologies in low-resource settings
- Environmental exposures affecting reproduction
- Reproductive health disparities in minority populations
- Digital health interventions in maternal care
- Blockchain for reproductive health records
- Ethical concerns in reproductive research
- Male contraception development
- Global reproductive health crises
- Impact of climate change on reproductive outcomes
- Reproductive health misinformation online
- Hormone therapy for transgender reproductive care
- Cross-cultural reproductive ethics
- Assisted reproduction in advanced maternal age
- Virtual reality in reproductive health education
- Innovative contraception technologies
- Social determinants and reproductive health
- Legal debates on reproductive autonomy
- Healthcare provider bias in reproductive care
- Public opinion and reproductive policy
- Reproductive health advocacy campaigns
How do reproductive health controversies impact health equity and patient care?
Reproductive health controversies have profound implications for both health equity and patient care. Access to reproductive services—including contraception, abortion, fertility treatments, and maternal care—is often influenced by social, economic, and political factors. Disparities in access disproportionately affect marginalized populations, including low-income individuals, rural communities, and racial and ethnic minorities. For instance, restrictive abortion laws in certain U.S. states have led to increased travel distances, delayed care, and higher risks for complications, illustrating a direct link between policy, service accessibility, and patient outcomes.
Nurses and other healthcare providers play a critical role in mitigating these inequities. They are often at the frontlines, providing care, education, and advocacy for patients navigating these systemic barriers. However, when controversies limit available services, nurses may encounter ethical and practical challenges in delivering high-quality, equitable care. For example, in regions where reproductive health clinics are scarce or legally restricted, patients may experience delayed prenatal care, increasing the risk of adverse maternal and neonatal outcomes. Similarly, inequitable access to fertility treatments raises ethical questions about fairness and distributive justice within the health system.
Reproductive health controversies also intersect with broader societal debates, such as the role of government funding in contraceptive access or Medicaid coverage for reproductive services. Policies that limit access to contraception or abortion disproportionately affect low-income patients, undermining health equity goals. Nurses must recognize how these structural issues influence individual patient experiences and outcomes and advocate for interventions that promote equitable care delivery.
What are the ethical issues around reproductive health services and health policy?
Ethical challenges in reproductive health arise from conflicts between patient autonomy, societal norms, legal restrictions, and professional responsibilities. Medical ethical principles—autonomy, beneficence, non-maleficence, and justice—provide a framework for evaluating these dilemmas. For instance, patients may seek services that are legally restricted in their region, creating tension between respecting patient confidentiality and adhering to legal mandates. Nurses may be called upon to navigate these conflicts, ensuring patients are informed of their options while safeguarding privacy and ethical standards.
Another ethical issue involves healthcare costs and the allocation of resources. Decisions about which reproductive services are covered under public insurance programs or employer plans can create disparities in who receives care. Limiting coverage for contraception or fertility treatments not only affects individual health outcomes but also raises questions about distributive justice and societal responsibility.
Health policy itself can create ethical dilemmas. For example, policies requiring mandatory counseling before abortion, or restricting telehealth reproductive services, may inadvertently coerce patient decision-making or limit timely access to care. Nurses must be prepared to advocate for policies that respect patient autonomy and promote equitable access while navigating institutional constraints.
Reproductive health services also involve sensitive issues such as informed consent for adolescents, access for LGBTQ+ individuals, and culturally appropriate care. Nurses must balance ethical obligations to provide evidence-based, patient-centered care with respect for diverse values and beliefs. For instance, providing reproductive health counseling for minors without parental involvement may be legally permissible but ethically complex, requiring careful consideration of the patient’s maturity, understanding, and best interests.
How do issues in healthcare and the health system influence access and equity?
Issues in healthcare and structural aspects of the healthcare system directly shape access to care and the equitable distribution of resources. Geographic location, socioeconomic status, and systemic biases all influence whether patients can receive timely, high-quality healthcare services. For instance, rural communities often face shortages of providers and limited access to specialty care, which can delay diagnosis and treatment, ultimately affecting health outcomes. Similarly, systemic inefficiencies—such as fragmented care coordination and underfunded facilities—disproportionately affect vulnerable populations, highlighting disparities in the health system.
Digital health innovations, while promising, also illustrate these challenges. Telehealth can expand reach, but patients without reliable internet or digital literacy may experience reduced access, raising questions about care quality and equity. Nursing students observing these disparities can better understand how organizational structures, policy decisions, and resource allocation influence patient care.
What health equity challenges exist within the health care system?
Health equity challenges in the health care system are multifaceted. Key issues include disparities in insurance coverage, inequitable distribution of providers, and differential access to preventive and specialty care. For example:
- Minority populations often experience higher maternal and infant mortality rates due to systemic barriers and implicit bias in care delivery.
- Patients with chronic conditions, such as diabetes or cardiovascular disease, may face fragmented care in under-resourced clinics, reducing care quality and continuity.
- Behavioral health services are frequently underfunded, leaving gaps for patients with mental health or substance use disorders, exacerbating disparities.
These inequities demonstrate that achieving high-quality care requires more than clinical competence; it necessitates systemic interventions, policy reform, and advocacy to ensure all patients can access care without discrimination.
How do healthcare costs and Medicare policies affect healthcare services?
Healthcare costs and Medicare policies are central determinants of access and equity. Rising costs can lead to delayed care, medication non-adherence, or avoidance of preventive services, particularly among low-income populations. For example, patients may skip essential screenings or follow-up visits due to high out-of-pocket expenses, negatively impacting health outcomes.
Medicare policies, including reimbursement rates and coverage limitations, shape the availability and scope of healthcare services. Hospitals and clinics may prioritize certain procedures or patient populations based on financial viability, which can create gaps in access. For instance, reductions in coverage for specific diagnostic tests or post-acute care services can disproportionately affect elderly or disabled patients, challenging the equitable delivery of care. Nursing students observing these policies can see how system-level decisions influence both organizational priorities and patient experiences.
What can nursing students learn about advocating for equitable health care services?
Nursing students have a unique vantage point to understand and address systemic inequities in the health care system. They can learn to:
- Recognize disparities: Understanding how social determinants, insurance status, and systemic barriers affect patient access helps nurses anticipate challenges in care delivery.
- Engage in patient advocacy: Nurses can help patients navigate insurance coverage, Medicare policies, and access barriers, ensuring they receive appropriate healthcare services.
- Promote policy awareness: Being informed about health policy and reimbursement structures enables nurses to advocate for equitable allocation of resources, such as preventive services and behavioral health programs.
- Support health education: Educating patients about available services, preventive care, and digital health tools can reduce inequities, particularly for underserved populations.
- Collaborate interprofessionally: Working with social workers, case managers, and community organizations can help address gaps in the health system and improve care quality.
For example, a nurse working in a community clinic may identify patients unable to afford transportation to specialty appointments and collaborate with local resources to facilitate access. By understanding these systemic influences, nursing students can develop skills in advocacy, equity-centered care, and ethical decision-making.
What controversies surround behavioral health and long-term care?
Behavioral health and long-term care are among the most debated areas in modern healthcare, with controversies spanning healthcare costs, service accessibility, treatment approaches, and regulatory oversight. Behavioral health controversies often revolve around the balance between patient autonomy and public safety, appropriate use of pharmacologic interventions, and disparities in access to mental health services. For example, there is ongoing debate about the overreliance on psychiatric medications versus the provision of psychotherapy or community-based interventions, especially in underfunded systems.
In long-term care, controversies frequently center on staffing levels, quality of care, and the allocation of limited resources in care facilities. Studies have shown that insufficient nurse-to-patient ratios in nursing homes can lead to increased incidence of pressure injuries, medication errors, and reduced care quality. Ethical debates also arise regarding residents’ autonomy versus protective oversight, particularly when cognitive impairments like dementia are present.
Funding models further complicate these issues. Medicare reimbursement policies may incentivize shorter hospital stays and discharge to long-term care facilities without sufficient preparation, raising concerns about patient safety and continuity of care. Meanwhile, the high cost of long-term care often creates inequities, disproportionately affecting older adults with limited financial resources or inadequate insurance coverage.
How do controversies in behavioral health impact healthcare providers and patient outcomes?
Controversies in behavioral health have direct consequences for both healthcare providers and patients. Clinicians often navigate conflicts between limited resources and patient needs. For instance, a patient with severe substance use disorder may require intensive inpatient rehabilitation, but insurance limitations or facility shortages can restrict access. This places ethical and professional strain on providers, who must prioritize care while attempting to uphold ethical standards.
Patient outcomes are also affected. Restricted access to evidence-based behavioral health services can result in worsening mental health, increased hospital readmissions, and greater risk of crises, such as self-harm or homelessness. Nurses may encounter moral distress when systemic barriers prevent them from delivering optimal high-quality care. Additionally, staffing shortages and high patient loads in behavioral health facilities can compromise patient monitoring, therapeutic engagement, and timely intervention.
Digital health innovations offer potential solutions but bring their own controversies. For example, telepsychiatry improves access for remote populations but raises concerns about privacy, security of patient information, and the quality of care compared to in-person interventions. Nursing students must understand how these evolving modalities influence both provider responsibilities and patient outcomes.
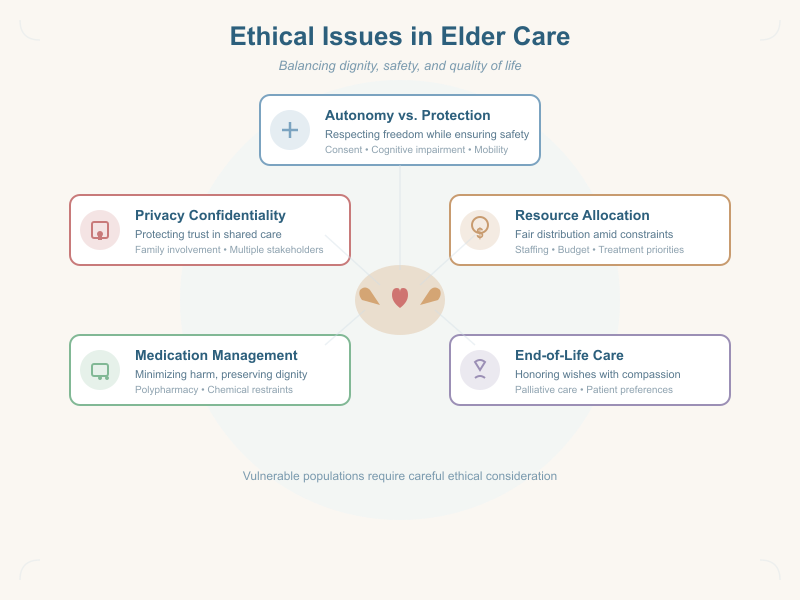
What ethical issues arise in long-term care and elder care settings?
Long-term care and elder care settings present unique ethical issues due to the vulnerability of residents and the complex interplay of autonomy, safety, and quality of life. Key dilemmas include:
- Autonomy vs. Protection: Elderly residents may have cognitive impairments that limit decision-making capacity. Nurses often face ethical decisions regarding consent for treatment, mobility restrictions, or participation in social activities, balancing patient safety with respect for personal freedom.
- Resource Allocation: Limited staffing, budget constraints, and facility resources raise ethical questions about fair distribution of care. Decisions about prioritizing treatments or allocating rehabilitation resources must consider both individual needs and systemic fairness.
- End-of-Life Care: Palliative care and assisted suicide debates are central ethical issues in elder care. Decisions about withdrawing or withholding interventions, pain management, and patient preferences require careful ethical deliberation guided by both medical ethics topics and institutional policies.
- Medication Management: Ethical concerns arise around polypharmacy, overprescription, and use of chemical restraints to manage behavioral symptoms in dementia. Nurses must advocate for approaches that minimize harm and respect dignity.
- Confidentiality and Privacy: Protecting patient information in long-term care, especially for residents with frequent family involvement, poses complex ethical challenges. Nurses must balance transparency with confidentiality, particularly when multiple stakeholders are involved.
For example, a resident with advanced dementia may refuse medication that is clinically indicated. Nurses and healthcare teams must navigate legal, ethical, and policy frameworks to determine the best course of action while prioritizing safety and dignity. Similarly, during staffing shortages, nurses must make difficult decisions about which residents require immediate attention, raising questions about care quality and ethical responsibility.
How is digital health changing conversations about medical controversies?
Digital health—including telemedicine, mobile health apps, wearable devices, and artificial intelligence (AI) in clinical decision-making—is reshaping debates around controversial medical topics. These technologies are expanding access to healthcare services, improving patient monitoring, and enabling remote care, but they also introduce new areas of uncertainty, risk, and ethical debate. For example, telehealth platforms have increased accessibility for reproductive health services, behavioral health consultations, and chronic disease management, but they raise questions about equity for patients without reliable internet access or digital literacy.
The integration of digital health tools has shifted conversations from traditional clinical controversies—such as procedural risks or treatment efficacy—to include debates about data security, algorithmic bias, and equitable access. Nursing students must understand how these tools both enable and complicate care delivery, preparing them to participate in discussions about evolving medical controversies.
What controversial medical topics emerge from digital health and health information use?
The use of health information systems, electronic health records (EHRs), and AI in patient care has generated several medical controversies. Key topics include:
- Algorithmic Bias: AI tools used for predictive diagnostics may inadvertently reflect existing healthcare disparities, potentially misclassifying disease risk in minority populations.
- Data Ownership and Consent: Patients often do not fully understand how their health data are stored, shared, or used for research, raising concerns about autonomy and patient confidentiality.
- Telemedicine Limitations: While telehealth expands access, controversies exist regarding its effectiveness for complex assessments, especially in mental health or reproductive health care.
- Digital Health Inequities: Populations without smartphones or internet access may be excluded from digital interventions, highlighting systemic inequities in the health system.
- Cybersecurity Risks: High-profile breaches of health information have underscored vulnerabilities in EHR systems, leading to debates about the balance between technological innovation and patient safety.
For instance, a 2025 report noted that predictive AI used in ICU patient monitoring occasionally overestimated deterioration risk for Black patients, leading to unnecessary interventions. Such controversies underscore the ethical, clinical, and policy implications of digital health adoption.
How should healthcare professionals address privacy and ethical issues in digital health?
Healthcare professionals must integrate ethical standards and legal guidance when using digital health technologies. Key strategies include:
- Ensuring Informed Consent: Patients should understand how their patient information is collected, stored, and potentially shared, particularly in telehealth or mobile app platforms.
- Maintaining Confidentiality: Nurses and clinicians must apply the same rigorous privacy protections in digital contexts as in traditional care, including secure communication channels and encryption.
- Addressing Algorithmic Bias: Clinicians should be aware of limitations in AI tools, validate outputs against clinical judgment, and advocate for continuous improvement and fairness in digital systems.
- Promoting Equity: Providers should identify barriers to digital health access and implement solutions, such as community-based technology support or alternative service pathways.
- Ethical Documentation Practices: Accurate and transparent documentation in EHRs is crucial for patient safety, interprofessional communication, and ethical accountability.
What are the implications of digital health for medical practice and patient care?
The integration of digital health into medical practice has transformative implications for patient care:
- Improved Access and Monitoring: Remote monitoring devices allow clinicians to track vital signs, medication adherence, and behavioral health symptoms, enhancing proactive care.
- Enhanced Patient Engagement: Mobile health apps and patient portals enable individuals to participate actively in their care, potentially improving adherence and health outcomes.
- Data-Driven Decision-Making: Analytics and AI tools can identify trends, predict risk, and support clinical decisions, but require critical oversight to avoid overreliance on technology.
- Workflow Optimization: EHRs streamline documentation and interprofessional communication, freeing nurses and other healthcare professionals to focus on direct patient care.
- Emerging Ethical Responsibilities: Providers must balance efficiency gains with ethical considerations, ensuring that digital health enhances rather than compromises care quality and patient trust.
For example, telepsychiatry has enabled behavioral health interventions in underserved areas, reducing hospitalizations and improving continuity of care. Simultaneously, clinicians must address privacy concerns and ensure equitable access for patients lacking technology resources.
Conclusion
Controversial medical healthcare topics present complex challenges that shape the practice, ethics, and decision-making processes of healthcare providers across diverse settings. From reproductive health and behavioral health to long-term care and the evolving landscape of digital health, these controversies illuminate the delicate balance between patient autonomy, safety, equitable access, and care quality. Understanding the nuances of these debates is critical for nursing students, who will encounter both systemic and individual-level ethical dilemmas throughout their professional careers.
Issues in healthcare, including disparities in access, inequities in healthcare services, and the influence of health policy and Medicare regulations, directly affect health outcomes and patient experiences. Nurses play a pivotal role in advocating for equitable care, applying ethical standards, and navigating complex clinical environments where medical ethics topics intersect with real-world decision-making. For instance, ensuring informed consent in reproductive health services, addressing patient confidentiality in digital platforms, and maintaining high-quality care in long-term care facilities are all practical manifestations of ethical competence and professional responsibility.
Moreover, the rise of digital health technologies and health information systems is reshaping conversations around medical controversies. While offering opportunities for improved monitoring, patient engagement, and efficiency, these tools also introduce ethical dilemmas related to privacy, equity, and algorithmic bias. Nursing students must be prepared to critically evaluate these technologies, advocate for safe implementation, and ensure that patient-centered care remains at the forefront of practice.
Ultimately, engaging with controversial medical topics equips nursing students to become informed, ethically grounded, and proactive professionals. By understanding systemic inequities, policy implications, and the ethical dimensions of patient care, future nurses can not only deliver safe and high-quality care but also contribute to the advancement of a health system that is equitable, transparent, and responsive to the needs of all patients. Mastery of these topics fosters critical thinking, professional accountability, and a commitment to improving patient outcomes—qualities essential for the evolving role of nurses in 2026 and beyond.
Frequently Asked Questions
What is the biggest issue currently facing healthcare?
The biggest issue is access to affordable, high-quality care, compounded by rising healthcare costs, workforce shortages, and health inequities. Challenges like managing chronic diseases, addressing behavioral health needs, and integrating digital health solutions also impact patient outcomes and system efficiency.
What are some hot topics in nursing?
Hot topics include:
- Nursing shortages and workforce sustainability
- Nurse burnout and mental health
- Telehealth and digital health adoption
- Patient safety and error prevention
- Health equity and access to care
- Ethical decision-making in clinical practice
- Reproductive and behavioral health care
- Long-term care and elder care challenges
- Advances in evidence-based practice
- Integration of AI and technology in nursing practice
What are the 10 ethical issues in medical assisting?
Common ethical issues include:
- Patient confidentiality and HIPAA compliance
- Informed consent for procedures
- Scope of practice violations
- Professional boundaries with patients
- Handling errors and reporting medical mistakes
- Conflict of interest in treatment recommendations
- Respecting patient autonomy and choices
- Equitable treatment across diverse populations
- Accurate documentation and honest record-keeping
- Compliance with laws and institutional policies
What are the debate topics for nursing?
Examples of debated nursing topics include:
- Mandatory vaccination for healthcare workers
- Nurse-to-patient staffing ratios
- Use of telehealth versus in-person care
- Assisted suicide and end-of-life decisions
- Ethical allocation of scarce resources
- Reproductive health rights and access
- Integration of AI in patient care
- Workplace safety and nurse burnout
- Cultural competence in care delivery
- Balancing patient autonomy with safety
